|
Colon Cancer Self
Test
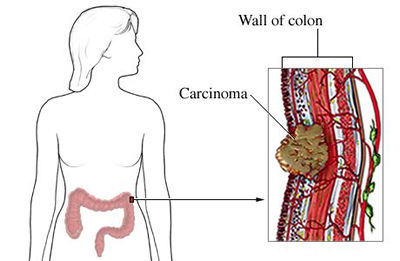
Colon (colorectal) cancer is
often called the "silent killer" Colon cancer affects both men and women
about equally and kills more people annually than either breast cancer or
prostate cancer.
Some reasons: neglect, lack of awareness, lack of media attention,
embarrassment, the "yuck" factor, too few people taking an active role in
monitoring their own health to prevent this disease.
Whatever the reason, the good news is that no one has to die from colon cancer.
With over a 90 percent cure rate caught early enough, colon cancer is
preventable and treatable. Early detection through screening is the key.
Colon cancer deaths could be nearly eliminated if most people learn the basics,
talk to their family and physicians about it, and take action to prevent it.
Unfortunately, as recent government surveys and studies show, less than 40% of
people who should be screened have been screened. Respondents age 50 and over to
a recent survey on this site said only 51% of their doctors discussed colon
cancer screening with them.
Prevention of colon cancer and other digestive disorders starts with you. It
requires that you take an active role in your own health. That means know the
basics:-
-
The early warning signs and
symptoms of colon cancer
-
Whether you have a family
history of cancer requiring earlier screening measures than the average
population
-
The different screening methods
available
-
The best screening tests to use
Although colon cancer can strike
with no warning signs, one of the most frequent and commonly the only early
warning sign is blood in your stool from bleeding polyps. Too often this sign is
either not noticed because the blood is not visible to the human eye or not
acted upon.
A healthy, normal individual does not bleed internally. If you do bleed
internally, resulting in either occult (hidden) or visible traces of blood in
stool, this can be a sign of colon cancer or other digestive health problem that
requires immediate medical attention
Recognise the difference between Ulcerative
Colitis and Colon Cancer
What Is Ulcerative Colitis?
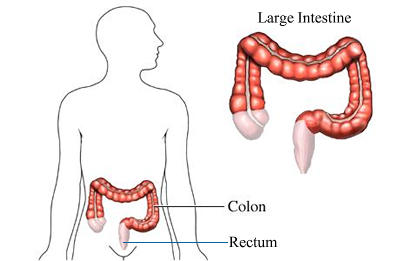
Ulcerative colitis is a condition that affects the large
intestine - the rectum and colon. It may affect only a part of the large
intestine, or the entire colon and rectum. Rarely, it may affect the last part
of the small intestine, called the ileum.
The affected part of the large intestine becomes inflamed and
develops ulcers, causing symptoms that include bloody diarrhoea, abdominal pain,
and fever.
Inflammation is the body's response to irritation or injury.
Inflammation causes tissues of the affected part of the body to become swollen,
red, warm, and painful. It is not known exactly what causes the bowel to become
inflamed.
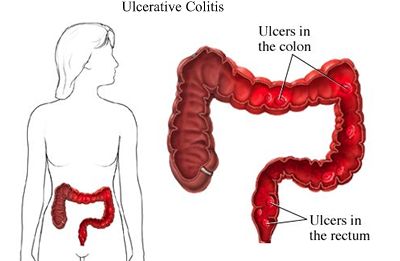
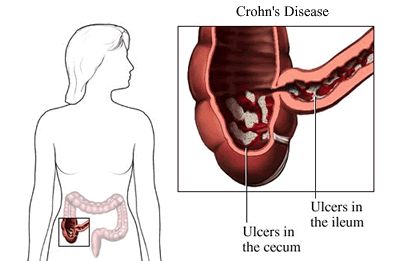
It is actually only the inner lining of the large bowel that
is affected in ulcerative colitis. A similar condition, Crohn's disease, can
cause inflammation in any portion of the gastrointestinal tract and can affect
the full thickness of the bowel wall. Both conditions, ulcerative colitis and
Crohn's disease, are known as inflammatory bowel disease.
In ulcerative colitis, the inflammation usually starts at the
rectum and ends at some point in the colon. The affected area is "continuous,"
that is, there is no area of normal tissue between the affected areas. The
amount of colon involved determines the classification of the type of ulcerative
colitis:
- Ulcerative proctitis
- ulcerative colitis that involves only the rectum
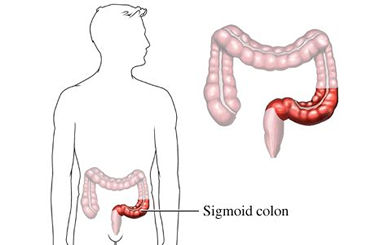
- Proctosigmoiditis
- ulcerative colitis that involves the rectum and sigmoid colon
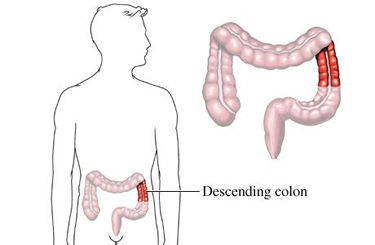
- Left-sided colitis
- ulcerative colitis that affects the entire left side of the colon: the
rectum, sigmoid colon, and descending colon
- Pancolitis -
ulcerative colitis that involves the entire colon
Symptoms of ulcerative colitis can be mild to severe and have
no relation to how much of the colon is affected. The condition is characterized
by periods of active disease, known as flare-ups, followed by periods when the
disease is inactive, known as remission
Q: What is the difference between ulcerative colitis and
Crohn's disease?
A: In both conditions there is inflammation of the intestine.
But ulcerative colitis affects just the colon, while Crohn's can affect any
portion of the gastrointestinal tract. Also, ulcerative colitis affects the
inner lining only, while Crohn's can affect the full thickness of the bowel
wall.
Some individuals suffer a single episode of ulcerative colitis
and never experience another flare-up. Others suffer frequent
flare-ups. For many people, flare-ups can be brought under control by a
combination of medication and dietary changes. For some, a period of complete
bowel rest and intravenous feeding is necessary.
Occasionally, removal of the entire colon - a total
colectomy - is necessary to deal with repeated, debilitating flare-ups,
or rarely, if colon cancer or precancerous changes occur. Removal of the colon
cures ulcerative colitis.
Remission and relapse
Remission refers to the period of time between flare-ups when
an individual is feeling relatively well. Although ulcerative colitis is a
chronic (ongoing) inflammatory bowel disease, it is characterized by remissions
that last for varying amounts of time, interrupted by acute flare-ups of
disease.
Each individual's pattern of symptoms is different, and
conscientious doctors treat the symptoms rather than the laboratory or
radiological signs.
Diarrhoea, pain, and fever - along with fatigue, chills, and
possibly vomiting - come and go. Flare-ups can occur seemingly out of the blue,
after a viral illness such as a cold, or at times of extreme personal, business,
or social stress
|