|
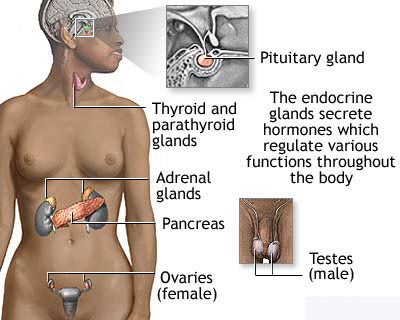
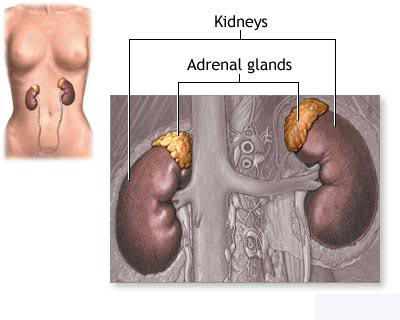
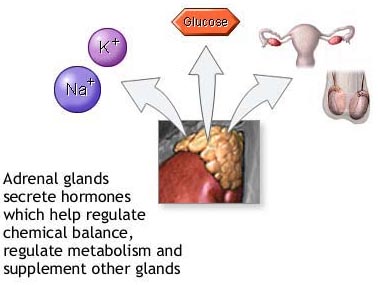
Adrenocortical Carcinoma
Cancer of the adrenal cortex, a rare
cancer, is a disease in which malignant cells are found in the adrenal cortex,
which is the outside layer of the adrenal gland. Cancer of the adrenal cortex is
also called adrenocortical carcinoma. There are two adrenal glands, one above
each kidney in the back of the upper abdomen. The adrenal glands are also called
the suprarenal glands. The inside layer of the adrenal gland is called the
adrenal medulla. Cancer that starts in the adrenal medulla is called
pheochromocytoma.
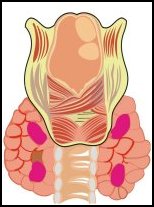
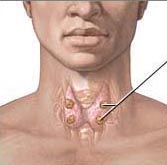
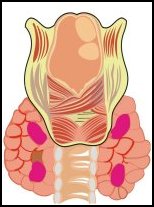
The four parathyroid glands
The parathyroid are a set of
four small glands located at the base of the neck, close to the thyroid
gland, either in its substance, or along its posterior surface, or very
close to it.
The parathyroid are involved in maintaining calcium metabolism, and they
do this with the help of a hormone they produce called parathyroid hormone
(PTH). The cells in the adrenal cortex make
important hormones that help the body work properly. When cells in the adrenal
cortex become cancerous, they may make too much of one or more hormones, which
can cause symptoms such as high blood pressure, weakening of the 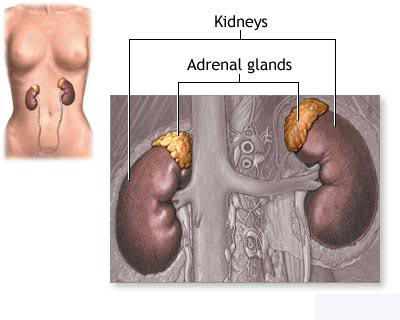 bones, or
diabetes. If male or female hormones are affected, the body may go through
changes such as a deepening of the voice, growing hair on the face, swelling of
the sex organs, or swelling of the breasts. Cancers that make hormones are
called functioning tumours. Many cancers of the adrenal cortex do not make extra
hormones and are called non-functioning tumours. bones, or
diabetes. If male or female hormones are affected, the body may go through
changes such as a deepening of the voice, growing hair on the face, swelling of
the sex organs, or swelling of the breasts. Cancers that make hormones are
called functioning tumours. Many cancers of the adrenal cortex do not make extra
hormones and are called non-functioning tumours.
A doctor should be seen if the following
symptoms appear and wonít go away:
- pain in the abdomen,
- loss of weight without
dieting
- weakness.
If there is a functioning
tumour, there may be symptoms or signs caused by too many hormones. If there are
symptoms, a doctor will order blood and urine tests to see whether the amounts
of hormones in the body are normal. A doctor may also order a computed
tomography scan of your abdomen, a special x-ray that uses a computer to make a
picture of the inside of the abdomen. Other special x-rays may also be done to
tell what kind of tumour is present.
The chance of recovery (prognosis)
depends on how far the cancer has spread (stage) and on whether a doctor was
able to surgically remove all of the cancer.
How cancer of the adrenal
cortex is treated
There are treatments for all patients
with cancer of the adrenal cortex. Three kinds of treatment are used:
-
Surgery (taking out the
cancer).
-
Chemotherapy (using drugs
to kill cancer cells).
-
Radiation therapy (using
high-dose x-rays or other high-energy rays to kill cancer cells).
A doctor may take out the adrenal gland
in an operation called an adrenalectomy. Tissues around the adrenal glands that
contain cancer may be removed. Lymph nodes in the area may also be removed
(lymph node dissection).
Chemotherapy uses drugs to kill cancer
cells. Chemotherapy may be taken by pill, or it may be put into the body by a
needle in a vein or muscle. Chemotherapy is called a systemic treatment because
the drug enters the bloodstream, travels through the body, and kills cancer
cells throughout the body.
Radiation therapy uses high-energy
x-rays to kill cancer cells and shrink tumours. Radiation for cancer of the
adrenal cortex usually comes from a machine outside the body (external radiation
therapy).
Besides treatment for cancer
(chemotherapy, radiation therapy, and/or surgery), a patient may also receive
therapy to prevent or treat symptoms caused by the extra hormones that are made
by the cancer.
BACK
|
|
Carcinoid
Tumour Gastrointestinal carcinoid
tumours are cancers in which malignant cells are found in certain hormone-making
cells of the digestive, or gastrointestinal, system. The digestive system
absorbs vitamins, minerals, carbohydrates, fats, proteins, and water from the
food that is eaten and stores waste until the body eliminates it. The digestive
system is made up of the stomach and the small and large intestines. The last 6
feet of intestine is called the colon. The last 10 inches of the colon is the
rectum. The appendix is an organ attached to the large intestine.
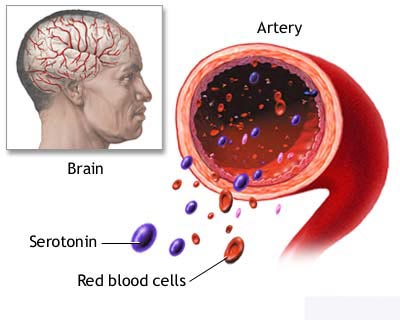
Carcinoid syndrome is the
pattern of symptoms that typically are exhibited by people with carcinoid
tumours. The symptoms include bright red facial flushing, diarrhoea, and
occasionally wheezing. A specific type of heart valve damage can occur, as well
as other cardiac problems. Carcinoid tumours secrete excessive amounts of the
hormone serotonin. Surgery with complete removal of the tumour tissue is the
ideal treatment. It can result in a permanent cure if it is possible to remove
the tumour entirely.
There are often no signs of a
gastrointestinal carcinoid tumour in its early stages. Often the cancer will
make too much of some of the hormones, which can cause symptoms. A doctor should
be seen if the following symptoms persist:
- Pain in the
abdomen.
- Flushing and
swelling of the skin of the face and neck.
- Wheezing.
- Diarrhoea.
- Symptoms of
heart failure, including breathlessness.
If there are symptoms, a doctor
may order blood and urine tests to look for signs of cancer. Other tests may
also be done. If there is a carcinoid tumour, the patient has a greater chance
of getting other cancers in the digestive system, either at the same time or at
a later time.
The chance of recovery
(prognosis) and choice of treatment depend on whether the cancer is just in the
gastrointestinal system or has spread to other places, and on the patient's
general state of health. There are treatments for all
patients with gastrointestinal carcinoid tumours. Four kinds of treatment are
used:
- Surgery (taking
out the cancer).
- Radiation
therapy (using high-dose x-rays to kill cancer cells).
- Biological
therapy (using the body's natural immune system to fight cancer).
- Chemotherapy
(using drugs to kill cancer cells).
Depending on where the cancer
started, the doctor may take out the cancer using one of the following
operations:
- A simple
appendectomy removes the appendix. If part of the colon is also taken out, the
operation is called a hemicolectomy. The doctor may also remove lymph nodes
and look at them under a microscope to see if they contain cancer.
- Local excision
uses a special instrument inserted into the colon or rectum through the anus
to cut the tumour out. This operation can be used for very small tumours.
- Fulguration uses
a special tool inserted into the colon or rectum through the anus. An electric
current is then used to burn the tumour away.
- Bowel resection
takes out the cancer and a small amount of healthy tissue on either side. The
healthy parts of the bowel are then sewn together. The doctor will also remove
lymph nodes and have them looked at under a microscope to see if they contain
cancer.
- Cryosurgery
kills the cancer by freezing it.
- Hepatic artery
ligation cuts and ties off the main blood vessel that brings blood into the
liver (the hepatic artery).
- Hepatic artery
embolization uses drugs or other agents to reduce or block the flow of blood
to the liver in order to kill cancer cells growing in the liver.
Radiation therapy uses
high-energy x-rays to kill cancer cells and shrink tumours. Radiation may come
from a machine outside the body (external radiation therapy) or from putting
materials that produce radiation (radioisotopes) through thin plastic tubes in
the area where the cancer cells are found (internal radiation therapy).
Chemotherapy uses drugs to kill
cancer cells. Chemotherapy may be taken by pill, or it may be put into the body
by a needle in the vein or muscle. Chemotherapy is called a systemic treatment
because the drug enters the bloodstream, travels through the body, and can kill
cancer cells outside the digestive system.
Biological therapy tries to get
the patient's body to fight the cancer. It uses materials made by the body or
made in a laboratory to boost, direct, or restore the body's natural defences
against disease. Biological therapy is sometimes called biological response
modifier (BRM) therapy or immunotherapy.
Treatment by type
Treatment of gastrointestinal
carcinoid tumour depends on the type of tumour, the stage, and the patient's
overall health.
Standard treatment may be
considered because of its effectiveness in patients in past studies, or
participation in a clinical trial may be considered. Not all patients are cured
with standard therapy and some standard treatments may have more side effects
than are desired. For these reasons, clinical trials are designed to find better
ways to treat cancer patients and are based on the most up-to-date information.
Localized
Gastrointestinal Carcinoid tumours
If the cancer started in the
appendix, the treatment will probably be surgery to remove the appendix
(appendectomy) with or without removal of part of the colon (hemicolectomy) and
lymph nodes.
If the cancer started in the
rectum, treatment will probably be simple surgery to remove the cancer, surgery
using electric current to burn the cancer away, surgery to remove part of the
rectum, or surgery to remove the anus and part of the rectum. An opening will be
made for waste to pass out of the body (colostomy) into a disposable bag
attached near the colostomy (colostomy bag).

If the cancer started in the
small intestine, the treatment will probably be surgery to remove part of the
bowel (bowel resection). Lymph nodes may also be taken out and looked at under
the microscope to see if they contain cancer.
If the cancer started in the
stomach, pancreas, or colon, the treatment will probably be surgery to remove
the organ affected by the cancer and possibly other nearby organs.
Regional
Gastrointestinal Carcinoid tumours
The treatment will probably be
surgery to remove the organ affected by the cancer and possibly other nearby
organs.
Metastatic
Gastrointestinal Carcinoid tumours
Treatment may be one of the
following:
- Surgery to
relieve symptoms caused by the cancer. Surgery to freeze and kill the cancer
may also be performed.
- Chemotherapy to
relieve symptoms caused by the cancer.
- Chemotherapy
injected directly into the hepatic artery to block the artery and kill cancer
cells growing in the liver.
- Radiation
therapy to relieve symptoms caused by the cancer.
- Radioactive
substances injected into the cancer to relieve the symptoms caused by the
cancer.
- Biological or
immunological therapy.
Carcinoid syndrome
Treatment options for
metastatic carcinoid tumour may be one of the following:
- Surgery to
remove the cancer.
- Surgery to cut
and tie the main artery that goes to the liver (hepatic artery ligation) or
injecting chemotherapy into the liver through the hepatic artery to block the
artery and kill cancer cells growing in the liver.
- Drugs designed
to relieve symptoms caused by the cancer.
- Biological
therapy to relieve symptoms caused by the cancer.
- A clinical trial
of new combinations of chemotherapy drugs.
BACK
|
|
Islet Cell
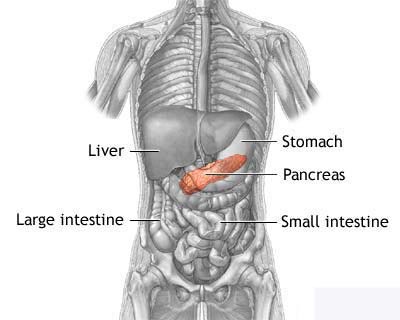
Carcinoma Islet cell cancer, a rare cancer, is a
disease in which malignant cells are found in certain tissues of the pancreas.
The pancreas is about 6 inches long and is shaped like a thin pear, wider at one
end and narrower at the other. The pancreas lies behind the stomach, inside a
loop formed by part of the small intestine. The broader right end of the
pancreas is called the head, the middle section is called the body, and the
narrow left end is the tail.
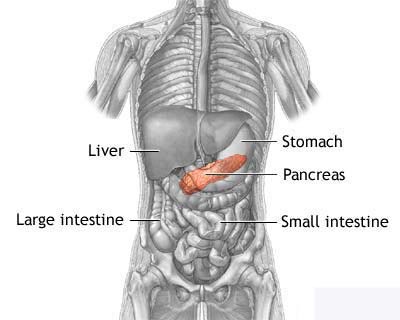 The pancreas has two basic jobs in
the body. It produces digestive juices that help break down (digest) food, and
hormones (such as insulin) that regulate how the body stores and uses food. The
area of the pancreas that produces digestive juices is called the exocrine
pancreas. About 95% of pancreatic cancers begin in the exocrine pancreas. The
hormone-producing area of the pancreas has special cells called islet cells and
is called the endocrine pancreas. Only about 5% of pancreatic cancers start
here. The pancreas has two basic jobs in
the body. It produces digestive juices that help break down (digest) food, and
hormones (such as insulin) that regulate how the body stores and uses food. The
area of the pancreas that produces digestive juices is called the exocrine
pancreas. About 95% of pancreatic cancers begin in the exocrine pancreas. The
hormone-producing area of the pancreas has special cells called islet cells and
is called the endocrine pancreas. Only about 5% of pancreatic cancers start
here.
The islet cells in the pancreas make
many hormones, including insulin, which help the body store and use sugars. When
islet cells in the pancreas become cancerous, they may make too many hormones.
Islet cell cancers that
 make too many hormones are called functioning tumours.
Other islet cell cancers may not make extra hormones and are called
non-functioning tumours. Tumours that do not spread to other parts of the body
can also be found in the islet cells. A doctor will need to determine whether the tumour is cancer or a
benign tumour. make too many hormones are called functioning tumours.
Other islet cell cancers may not make extra hormones and are called
non-functioning tumours. Tumours that do not spread to other parts of the body
can also be found in the islet cells. A doctor will need to determine whether the tumour is cancer or a
benign tumour.
A doctor should be seen if there is pain
in the abdomen, diarrhoea, stomach pain, a tired feeling all the time, fainting,
or weight gain without eating too much.
If there are symptoms, the doctor will
order blood and urine tests to see whether the amounts of hormones in the body
are normal. Other tests, including x-rays and special scans, may also be done.
The chance of recovery (prognosis)
depends on the type of islet cell cancer the patient has, how far the cancer has
spread, and the patientís overall health.
Stages of islet cell cancer
Once islet cell cancer is found, more
tests will be done to find out if cancer cells have spread to other parts of the
body. This is called staging. The staging system for islet cell cancer is still
being developed. These tumours are most often divided into one of three groups:
- islet cell cancers
occurring in one site within the pancreas,
- islet cell cancers
occurring in several sites within the pancreas, or
- islet cell cancers that
have spread to lymph nodes near the pancreas or to distant sites.
A doctor also needs to know the type of
islet cell tumour to plan treatment. The following types of islet cell tumours
are found:
Gastrinoma
The tumour makes large amounts of a
hormone called gastrin, which causes too much acid to be made in the stomach.
Ulcers may develop as a result of too much stomach acid.
Insulinoma
The tumour makes too much of the hormone
insulin and causes the body to store sugar instead of burning the sugar for
energy. This causes too little sugar in the blood, a condition called
hypoglycaemia.
Glucagonoma
This tumour makes too much of the
hormone glucagon and causes too much sugar in the blood, a condition called
hyperglycaemia.
Miscellaneous
Other types of islet cell cancer can
affect the pancreas and/or small intestine. Each type of tumour may affect
different hormones in the body and cause different symptoms.
Recurrent
Recurrent disease means that the cancer
has come back (recurred) after it has been treated. It may come back in the
pancreas or in another part of the body.
How islet cell cancer is
treated
There are treatments for all patients
with islet cell cancer. Three types of treatment are used:
- Surgery (taking out the
cancer).
- Chemotherapy (using drugs
to kill cancer cells).
- Hormone therapy (using
hormones to stop cancer cells from growing).
Surgery is the most common treatment of
islet cell cancer. The doctor may take out the cancer and most or part of the
pancreas. Sometimes the stomach is taken out (gastrectomy) because of ulcers.
Lymph nodes in the area may also be removed and looked at under a microscope to
see if they contain cancer.
Chemotherapy uses drugs to kill cancer
cells. Chemotherapy may be taken by pill, or it may be put into the body by a
needle in the vein or muscle. Chemotherapy is called a systemic treatment
because the drug enters the bloodstream, travels through the body, and can kill
cancer cells throughout the body.
Hormone therapy uses hormones to stop
the cancer cells from growing or to relieve symptoms caused by the tumour.
Hepatic arterial occlusion or
embolization uses drugs or other agents to reduce or block the flow of blood to
the liver in order to kill cancer cells growing in the liver.
Gastrinoma
Treatment may be one of the following:
- Surgery to remove the
cancer.
- Surgery to remove the
stomach (gastrectomy).
- Surgery to cut the nerve
that stimulates the pancreas.
- Chemotherapy.
- Hormone therapy.
- Hepatic arterial
occlusion or embolization to kill cancer cells growing in the liver.
Insulinoma
Treatment may be one of the following:
- Surgery to remove the
cancer.
- Chemotherapy.
- Hormone therapy.
- Drugs to relieve
symptoms.
- Hepatic arterial
occlusion or embolization to kill cancer cells growing in the liver.
Glucagonoma
Treatment may be one of the following:
- Surgery to remove the
cancer.
- Chemotherapy.
- Hormone therapy.
- Hepatic arterial
occlusion or embolization to kill cancer cells growing in the liver.
Miscellaneous Islet Cell
Cancer
Treatment may be one of the following:
- Surgery to remove the
cancer.
- Chemotherapy.
- Hormone therapy.
- Hepatic arterial
occlusion or embolization to kill cancer cells growing in the liver.
BACK
|
|
Parathyroid Cancer
Parathyroid cancer, a very rare
cancer, is a disease in which malignant cells are found in the tissues of the
parathyroid gland. The parathyroid gland is at the base of the neck, near the
thyroid gland. The parathyroid gland makes a hormone called parathyroid hormone
(PTH), or parathormone, which helps the body store and use calcium.
Problems with the parathyroid
gland are common and are usually not caused by cancer. If parathyroid cancer is
found, the parathyroid gland may be making too much PTH. This causes too much
calcium to be found in the blood. The extra PTH also takes calcium from the
bones, which causes pain in the bones, kidney problems, and other types of
problems. There are other conditions that can cause the parathyroid gland to
make too much PTH. It is important for a doctor to determine what is causing the
extra PTH. Hyperparathyroidism is a condition which can cause the body to make
extra PTH. If hyperparathyroidism runs in the family, there is a greater chance
of getting this type of cancer.
A doctor should be seen if
there are the following symptoms: bone pain, a lump in the neck, pain in the
upper part of the back, weak muscles, difficulty speaking, or vomiting.
If there are symptoms, the
doctor will conduct a physical examination and feel for lumps in the throat. The
doctor may also order blood tests and other tests to check for cancer or other
types of tumours that may not be cancer (benign tumours).
The chance of recovery
(prognosis) depends on whether the cancer is just in the parathyroid gland or
has spread to other parts of the body (stage) and the patientís general health.
How parathyroid cancer is
treated
There are treatments for all
patients with parathyroid cancer. Two kinds of treatment are used:
- Surgery (taking
out the cancer).
- Radiation
therapy (using high-dose x-rays or other high-energy rays to kill cancer
cells).
Surgery is the most common
treatment of parathyroid cancer. A doctor may remove the parathyroid gland (parathyroidectomy)
and the half of the thyroid on the same side as the cancer (ipsilateral
thyroidectomy).
Radiation therapy uses
high-energy x-rays to kill cancer cells and shrink tumours. Radiation may come
from a machine outside the body (external radiation therapy) or from putting
materials that produce radiation (radioisotopes) through thin plastic tubes in
the area where the cancer cells are found (internal radiation therapy).
Chemotherapy (using drugs to
kill cancer cells) is being studied in clinical trials. Chemotherapy uses drugs
to kill cancer cells. Chemotherapy may be taken by pill, or it may be put into
the body by a needle in the vein or muscle. Chemotherapy is called a systemic
treatment because the drug enters the bloodstream, travels through the body, and
can kill cancer cells outside the parathyroid gland.
Localized
Parathyroid Cancer
Treatment may be one of the
following:
- Surgery to
remove the parathyroid gland (parathyroidectomy) and the half of the thyroid
on the same side as the cancer (ipsilateral thyroidectomy).
- A clinical trial
of surgery followed by radiation therapy.
- A clinical trial
of radiation therapy.
Metastatic
Parathyroid Cancer
Treatment may be one of the
following:
- Surgery to
remove the parathyroid gland (parathyroidectomy) and other tissues around the
thyroid if they contain cancer.
- Surgery to
remove as much of the parathyroid gland as possible in order to reduce
production of PTH.
- Medical
treatment to reduce the amount of calcium in the blood.
- A clinical trial
of surgery followed by radiation therapy.
- A clinical trial
of radiation therapy.
- A clinical trial
of chemotherapy.
Recurrent
Parathyroid Cancer
Recurrent disease can occur as
late as 34 years after the first tumour.
Treatment may be one of the
following:
- Surgery to
remove the parathyroid gland (parathyroidectomy) and other tissues around the
thyroid if they contain cancer.
- Surgery to
remove as much of the parathyroid gland as possible in order to reduce
production of PTH.
- Medical
treatment to reduce the amount of calcium in the blood.
- A clinical trial
of surgery followed by radiation therapy.
- A clinical trial
of radiation therapy.
- A clinical trial
of chemotherapy.
BACK
|
|
Pheochromocytoma Pheochromocytoma, a rare
cancer, is a disease in which malignant cells are found in special cells in the
body called chromaffin cells. Most pheochromocytomas start inside the adrenal
gland (the adrenal medulla) where most chromaffin cells are located. There are
two adrenal glands, one above each kidney in the back of the upper abdomen.
Cells in the adrenal glands make important hormones that help the body work
properly. Usually pheochromocytoma affects only one adrenal gland.
Pheochromocytoma may also start in other parts of the body, such as the area
around the heart or bladder. 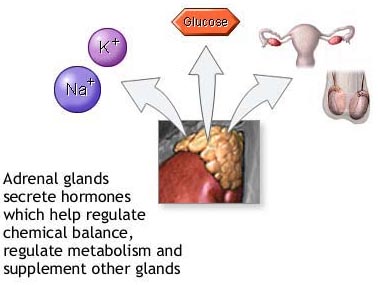
Most tumours that start in the
chromaffin cells do not spread to other parts of the body and are not cancer. If
a tumour is found, the doctor will need to determine whether it is cancer or
benign.
Pheochromocytomas often cause
the adrenal glands to make too many hormones called catecholamines. The extra
catecholamines cause high blood pressure (hypertension), which can cause
headaches, sweating, pounding of the heart, pain in the chest, and a feeling of
anxiety. High blood pressure that goes on for a long time without treatment can
lead to heart disease, stroke, and other major health problems.
If there are symptoms, a doctor
may order blood and urine tests to see if there are extra hormones in the body.
A patient may also have a special nuclear medicine scan. A CT scan, an x-ray
that uses a computer to make a picture of the inside of a part of the body or an
MRI scan, which uses magnetic waves to make a picture of the abdomen, may also
be done.
Pheochromocytoma is sometimes
part of a condition called multiple endocrine neoplasia syndrome (MEN). People
with MEN often have other cancers (such as thyroid cancer) and other hormonal
problems. The chance of recovery
(prognosis) depends on how far the cancer has spread, and the patientís age and
general health.
Localized benign
pheochromocytoma
Tumour is found in only one
area and has not spread to other tissues. Most pheochromocytomas do not spread
to other parts of the body and are not cancer.
Regional pheochromocytoma
Cancer has spread to lymph
nodes in the area or to other tissues around the original cancer. (Lymph nodes
are small bean-shaped structures that are found throughout the body. They
produce and store infection-fighting cells.)
Metastatic pheochromocytoma
The cancer has spread to other
parts of the body.
Recurrent pheochromocytoma
Recurrent disease means that
the cancer has come back (recurred) after it has been treated. It may come back
in the area where it started or in another part of the body.
How pheochromocytoma is
treated
There are treatments for all
patients with pheochromocytoma. Three kinds of treatment are used:
- Surgery (taking
out the cancer).
- Radiation
therapy (using high-dose x-rays or other high-energy rays to kill cancer
cells).
- Chemotherapy
(using drugs to kill cancer cells).
Surgery is the most common
treatment of pheochromocytoma. A doctor may remove one or both adrenal glands in
an operation called adrenalectomy. The doctor will look inside the abdomen to
make sure all the cancer is removed. If the cancer has spread, lymph nodes or
other tissues may also be taken out.
Chemotherapy uses drugs to kill
cancer cells. Chemotherapy may be taken by pill, or it may be put into the body
by a needle in the vein or muscle. Chemotherapy is called a systemic treatment
because the drug enters the bloodstream, travels through the body, and can kill
cancer cells throughout the body.
Radiation therapy uses
high-energy x-rays to kill cancer cells and shrink tumours. Radiation comes from
a machine outside the body (external radiation therapy).
Localized Benign
Pheochromocytoma
Treatment will probably be
surgery to remove one or both adrenal glands (adrenalectomy). After surgery the
doctor will order blood and urine tests to make sure hormone levels return to
normal.
Regional
Pheochromocytoma
Treatment may be one of the
following:
- Surgery to
remove one or both adrenal glands (adrenalectomy) and as much of the cancer as
possible. If cancer remains after surgery, drugs will be given to control high
blood pressure.
- External
radiation therapy to relieve symptoms (in rare cases).
- Chemotherapy.
Metastatic
Pheochromocytoma
Treatment may be one of the
following:
- Surgery to
remove as much of the cancer as possible. If cancer remains after surgery,
drugs will be given to control high blood pressure.
- External
radiation therapy to relieve symptoms.
- Chemotherapy.
BACK
|
|
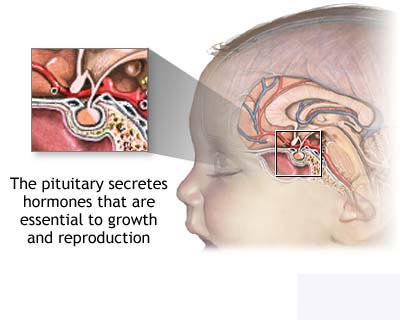
Pituitary Tumours
Pituitary tumours are tumours
found in the pituitary gland, a small organ about the size of a pea in the
centre of the brain just above the back of the nose. The pituitary gland makes
hormones that affect the growth and the functions of other glands in the body.
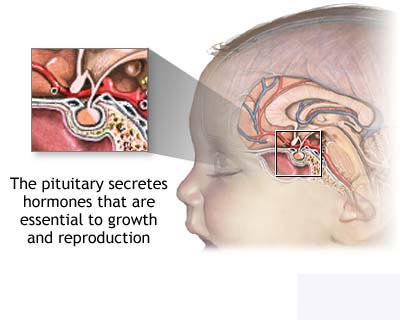 Most pituitary tumours
are benign. They grow very slowly and do not spread to other
parts of the body. If a pituitary tumour is found,
the pituitary gland may be making too many hormones. This can cause other
problems in the body. Tumours that make hormones are called functioning tumours,
while those that do not make hormones are called non-functioning tumours. Most pituitary tumours
are benign. They grow very slowly and do not spread to other
parts of the body. If a pituitary tumour is found,
the pituitary gland may be making too many hormones. This can cause other
problems in the body. Tumours that make hormones are called functioning tumours,
while those that do not make hormones are called non-functioning tumours.
Certain pituitary tumours can
cause a disease called Cushingís disease, in which too many hormones called
glucocorticoids are released into the bloodstream. This causes fat to build up
in the face, back, and chest, and the arms and legs to become very thin. Other
symptoms include too much sugar in the blood, weak muscles and bones, a flushed
face, and high blood pressure. Other pituitary tumours can cause a condition
called acromegaly. Acromegaly means that the hands, feet, and face are larger
than normal and in very young people, the whole body may grow much larger than
normal. Another type of pituitary tumour can cause the breasts to make milk,
even though a woman may not be pregnant, periods may stop as well.
A doctor should be seen if
there are symptoms such as:
- Headaches.
- Trouble seeing.
- Nausea or
vomiting.
- Any of the
symptoms caused by too many hormones.
If there are symptoms, a doctor
may order laboratory tests to see what the hormone levels are in the blood. The
doctor may also order an MRI (magnetic resonance imaging) scan, which uses
magnetic waves to make a picture of the inside of the brain. Other special
x-rays may also be done.
The prognosis (chance of
recovery) and choice of treatment depend on the type of tumour, and the patientís
age and general state of health.
Types of pituitary tumours
Once a pituitary tumour is
found, more tests will be done to find out how far the tumour has spread and
whether or not it makes hormones. A doctor needs to know the type of tumour to
plan treatment. The following types of pituitary tumours are found:
ACTH-producing tumours
These tumours make a hormone
called adrenocorticotropic hormone (ACTH), which stimulates the adrenal glands
to make glucocorticoids. When the body makes too much ACTH, it causes Cushingís
disease.
Prolactin-producing tumours
These tumours make prolactin, a
hormone that stimulates a womanís breasts to make milk during and after
pregnancy. Prolactin-secreting tumours can cause the breasts to make milk and
menstrual periods to stop when a woman is not pregnant. In men, prolactin-producing
tumours can cause impotence.
Growth hormone-producing
tumours
These tumours make growth
hormone, which can cause acromegaly or gigantism when too much is made.
Non-functioning pituitary
tumours
Non-functioning tumours do not
produce hormones.
How pituitary tumours are
treated
There are treatments for all
patients with pituitary tumours. Three kinds of treatment are used:
- Surgery
- Radiation
therapy (using high-dose x-rays to kill tumour cells).
- Drug therapy.
Surgery is a common treatment
of pituitary tumours. A doctor may remove the tumour using one of the following
operations:
- A
transsphenoidal hypophysectomy removes the tumour through a cut in the nasal
passage.
- A craniotomy
removes the tumour through a cut in the front of the skull.
Radiation therapy uses
high-energy x-rays to kill cancer cells and shrink tumours. Radiation for
pituitary tumours usually comes from a machine outside the body (external
radiation therapy). Radiation therapy may be used alone or in addition to
surgery or drug therapy.
Certain drugs can also block
the pituitary gland from making too many hormones.
ACTH-Producing
Pituitary Tumours
Treatment may be one of the
following:
- Surgery to
remove the tumour (transsphenoidal hypophysectomy or craniotomy
- Radiation
therapy. Clinical trials may be testing new types of radiation therapy.
- Surgery plus
radiation therapy.
- Radiation
therapy plus drug therapy to stop the tumour from making ACTH.
Prolactin-Producing
Pituitary Tumours
Treatment may be one of the
following:
- Surgery to
remove the tumour (transsphenoidal hypophysectomy or craniotomy).
- Radiation
therapy.
- Surgery,
radiation therapy, and drug therapy.
- Drug therapy to
stop the tumour from making prolactin. Clinical trials are testing new drugs
for this purpose.
Growth
Hormone-Producing Pituitary Tumours
Treatment may be one of the
following:
- Surgery to
remove the tumour (transsphenoidal hypophysectomy or craniotomy).
- Radiation
therapy.
- Drug therapy to
stop the tumour from making growth hormone.
Non-functioning
Pituitary Tumours
Treatment may be one of the
following:
- Surgery to
remove the tumour (transsphenoidal hypophysectomy or craniotomy).
- Radiation
therapy alone or in addition to surgery.
Recurrent
Pituitary Tumours
Treatment of recurrent
pituitary tumour depends on the type of tumour, the type of treatment the
patient has already had, and other factors such as the patientís general
condition. Patients may want to take part in a clinical trial of new treatments.
BACK
|
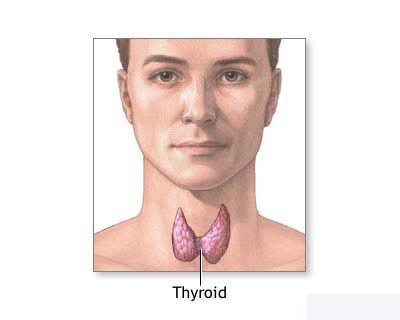
Thyroid Cancer
Cancer of the thyroid is a disease in which cancer cells are found in the
tissues of the thyroid gland. The thyroid gland is at the base of the throat. It
has two lobes, one on the right side and one on the left. The thyroid gland
makes important hormones that help the body function normally.
Cancer of the thyroid is more common in women than in men. Most patients are
between 25 and 65 years old. People who have been exposed to large amounts of
radiation, or who have had radiation treatment for medical problems in the head
and neck have a higher chance of getting thyroid cancer. The cancer may not
occur until 20 years or longer after radiation treatment.
A doctor should be seen if there is a lump or swelling in the front of the neck
or in other parts of the neck.
If there are symptoms, a doctor will feel the patientís thyroid and check for
lumps in the neck. The doctor may order blood tests and special scans to see
whether a lump in the thyroid is making too many hormones. The doctor may want
to take a small amount of tissue from the thyroid. This is called a biopsy. To
do this, a small needle is inserted into the thyroid at the base of the throat
and some tissue is drawn out. The tissue is then looked at under a microscope to
see whether it contains cancer.
There are four main types of cancer of the thyroid (based on how the cancer
cells look under a microscope):
- papillary
- follicular
- medullary
- anaplastic
The chance of recovery (prognosis) depends on the type of thyroid cancer,
whether it is just in the thyroid or has spread to other parts of the body
(stage), and the patientís age and overall health. Some types of thyroid cancer
grow much faster than others.
The genes in our cells carry the hereditary information from our parents. An
abnormal gene has been found in patients with some forms of thyroid cancer. If
medullary thyroid cancer is found, the patient may have been born with a certain
abnormal gene which may have led to the cancer. Family members may have also
inherited this abnormal gene. Tests have been developed to determine who has the
genetic defect long before any cancer appears. It is important that the patient
and his or her family members (children, grandchildren, parents, brothers,
sisters, nieces and nephews) see a doctor about tests that will show if the
abnormal gene is present. These tests are confidential and can help the doctor
help patients. Family members, including young children, who donít have cancer,
but do have this abnormal gene, may reduce the chance of developing medullary
thyroid cancer by having surgery to safely remove the thyroid gland (thyroidectomy).
Stages of cancer of the thyroid
Once cancer of the thyroid is found (diagnosed), more tests will be done to find
out if cancer cells have spread to other parts of the body. This is called
staging. A doctor needs to know the stage of the disease to plan treatment.
The following stages are used for papillary cancers of the thyroid:
Stage I papillary
Cancer is only in the thyroid and may be found in one or both lobes.
Stage II papillary
In patients younger than 45 years of age:
Cancer has spread beyond the thyroid.
In patients older than 45 years of age:
Cancer is only in the thyroid and larger than 1 centimetre (about 1/2 inch).
Stage III papillary
Cancer is found in patients older than 45 years of age and has spread outside
the thyroid (but not outside of the neck) or has spread to the lymph nodes.
Stage IV papillary
Cancer is found in patients older than 45 years of age and has spread to other
parts of the body, such as the lungs and bones.
The following stages are used for follicular cancers of the thyroid:
Stage I follicular
Cancer is only in the thyroid and may be found in one or both lobes.
Stage II follicular
In patients younger than 45 years of age:
Cancer has spread beyond the thyroid.
In patients older than 45 years of age:
Cancer is only in the thyroid and larger than 1 centimetre (about 1/2 inch).
Stage III follicular
Cancer is found in patients older than 45 years of age and has spread outside
the thyroid (but not outside of the neck) or to the lymph nodes.
Stage IV follicular
Cancer is found in patients older than 45 years of age and has spread to other
parts of the body, such as the lungs and bones.
Other types or stages of thyroid cancer include the following:
Stage I medullary
Cancer is less than 1 centimetre (about 1/2 inch) in size.
Stage II medullary
Cancer is between 1 and 4 centimetres (about 1/2 to 1 1/2 inches) in size.
Stage III medullary
Cancer has spread to the lymph nodes.
Stage IV medullary
Cancer has spread to other parts of the body.
Anaplastic
There is no staging system for anaplastic cancer of the thyroid. This type of
cancer of the thyroid grows faster than the other types.
Recurrent
Recurrent disease means that the cancer has come back (recurred) after it has
been treated. It may come back in the thyroid or in another part of the body.
How cancer of the thyroid is treated
There are treatments for all patients with cancer of the thyroid. Four types of
treatment are used:
Surgery (taking out the cancer).
Radiation therapy (using high-dose x-rays or other high-energy rays to kill
cancer cells).
Hormone therapy (using hormones to stop cancer cells from growing) .
Chemotherapy (using drugs to kill cancer cells).
Surgery is the most common treatment of cancer of the thyroid. A doctor may
remove the cancer using one of the following operations:
-
Lobectomy
removes only the side of the thyroid where the cancer is found.
Lymph nodes in the area may be taken out (biopsied) to see if
they contain cancer
-
Near-total thyroidectomy
removes all of the thyroid except for a small part
-
Total thyroidectomy
removes the entire thyroid
-
Lymph node
dissection removes lymph nodes in the neck that contain cancer
Radiation therapy uses high-energy x-rays to kill cancer cells and shrink
tumours. Radiation for cancer of the thyroid may come from a machine outside the
body (external radiation therapy) or from drinking a liquid that contains
radioactive iodine. Because the thyroid takes up iodine, the radioactive iodine
collects in any thyroid tissue remaining in the body and kills the cancer cells.
Hormone therapy uses hormones to stop cancer cells from growing. In treating
cancer of the thyroid, hormones can be used to stop the body from making other
hormones that might make cancer cells grow. Hormones are usually given as pills.
Chemotherapy uses drugs to kill cancer cells. Chemotherapy may be taken by pill,
or it may be put into the body by a needle in the vein or muscle. Chemotherapy
is called a systemic treatment because the drug enters the bloodstream, travels
through the body, and can kill cancer cells outside the thyroid.
Stage I Papillary Thyroid Cancer
Treatment may be one of the following:
Surgery to remove one lobe of the thyroid (lobectomy), followed by hormone
therapy. Radioactive iodine also may be given following surgery.
Surgery to remove the thyroid (total thyroidectomy).
Stage I Follicular Thyroid Cancer
Treatment may be one of the following:
Surgery to remove the thyroid (total thyroidectomy).
Surgery to remove one lobe of the thyroid (lobectomy), followed by hormone
therapy. Radioactive iodine also may be given following surgery.
Stage II Papillary Thyroid Cancer
Treatment may be one of the following:
Surgery to remove one lobe of the thyroid (lobectomy) and lymph nodes that
contain cancer, followed by hormone therapy. Radioactive iodine also may be
given following surgery.
Surgery to remove the thyroid (total thyroidectomy).
Stage II Follicular Thyroid Cancer
Treatment may be one of the
following:
Surgery to remove the thyroid (total thyroidectomy).
Surgery to remove one lobe of the thyroid (lobectomy) and lymph nodes that
contain cancer, followed by hormone therapy. Radioactive iodine also may be
given following surgery.
Stage III Papillary Thyroid Cancer
Treatment may be one of the following:
Surgery to remove the entire thyroid (total thyroidectomy) and lymph nodes where
cancer has spread.
Total thyroidectomy followed by radiation therapy with radioactive iodine or
external beam radiation therapy.
Stage III Follicular Thyroid Cancer
Treatment may be one of the following:
Surgery to remove the entire thyroid (total thyroidectomy) and lymph nodes or
other tissues around the thyroid where the cancer has spread.
Total thyroidectomy followed by radioactive iodine or external beam radiation
therapy.
Stage IV Papillary Thyroid Cancer
Treatment may be one of the following:
Radioactive iodine.
External beam radiation therapy.
Hormone therapy.
A clinical trial of chemotherapy.
Stage IV Follicular Thyroid Cancer
Treatment may be one of the following:
Radioactive iodine.
External beam radiation therapy.
Hormone therapy.
A clinical trial of chemotherapy.
Medullary Thyroid Cancer
Treatment will probably be surgery to remove the entire thyroid (total
thyroidectomy) unless the cancer has spread to other parts of the body. If lymph
nodes in the neck contain cancer, the lymph nodes in the neck will be removed
(lymph node dissection). If the cancer has spread to other parts of the body,
chemotherapy may be given.
Anaplastic Thyroid Cancer
Treatment may be one of the following:
Surgery to remove the thyroid and the tissues around it. Because this cancer
often spreads very quickly to other tissues, a doctor may have to take out part
of the tube through which a person breathes. The doctor will then make an airway
in the throat so the patient can breathe. This is called a tracheostomy.
Total thyroidectomy to reduce symptoms if the disease remains in the area of the
thyroid.
External beam radiation therapy.
Chemotherapy.
Clinical trials studying new methods of treatment of thyroid cancer.
Recurrent Thyroid Cancer
The choice of treatment depends on the type of thyroid cancer the patient has,
the kind of treatment the patient had before, and where the cancer comes back.
Treatment may be one of the following:
Surgery with or without radioactive iodine.
External beam radiation therapy to relieve symptoms caused by the cancer.
Chemotherapy.
Radioactive iodine.
Radiation therapy given during surgery.
Clinical trials.
BACK |


 bones, or
diabetes. If male or female hormones are affected, the body may go through
changes such as a deepening of the voice, growing hair on the face, swelling of
the sex organs, or swelling of the breasts. Cancers that make hormones are
called functioning tumours. Many cancers of the adrenal cortex do not make extra
hormones and are called non-functioning tumours.
bones, or
diabetes. If male or female hormones are affected, the body may go through
changes such as a deepening of the voice, growing hair on the face, swelling of
the sex organs, or swelling of the breasts. Cancers that make hormones are
called functioning tumours. Many cancers of the adrenal cortex do not make extra
hormones and are called non-functioning tumours. 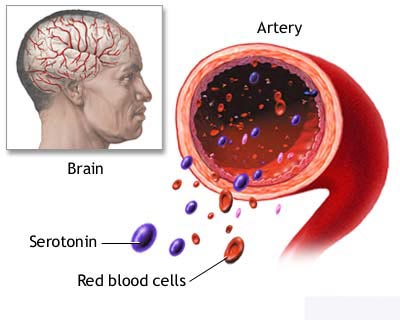

 The pancreas has two basic jobs in
the body. It produces digestive juices that help break down (digest) food, and
hormones (such as insulin) that regulate how the body stores and uses food. The
area of the pancreas that produces digestive juices is called the exocrine
pancreas. About 95% of pancreatic cancers begin in the exocrine pancreas. The
hormone-producing area of the pancreas has special cells called islet cells and
is called the endocrine pancreas. Only about 5% of pancreatic cancers start
here.
The pancreas has two basic jobs in
the body. It produces digestive juices that help break down (digest) food, and
hormones (such as insulin) that regulate how the body stores and uses food. The
area of the pancreas that produces digestive juices is called the exocrine
pancreas. About 95% of pancreatic cancers begin in the exocrine pancreas. The
hormone-producing area of the pancreas has special cells called islet cells and
is called the endocrine pancreas. Only about 5% of pancreatic cancers start
here.  make too many hormones are called functioning tumours.
Other islet cell cancers may not make extra hormones and are called
non-functioning tumours. Tumours that do not spread to other parts of the body
can also be found in the islet cells. A doctor will need to determine whether the tumour is cancer or a
benign tumour.
make too many hormones are called functioning tumours.
Other islet cell cancers may not make extra hormones and are called
non-functioning tumours. Tumours that do not spread to other parts of the body
can also be found in the islet cells. A doctor will need to determine whether the tumour is cancer or a
benign tumour. 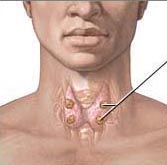
 Most pituitary tumours
are benign. They grow very slowly and do not spread to other
parts of the body. If a pituitary tumour is found,
the pituitary gland may be making too many hormones. This can cause other
problems in the body. Tumours that make hormones are called functioning tumours,
while those that do not make hormones are called non-functioning tumours.
Most pituitary tumours
are benign. They grow very slowly and do not spread to other
parts of the body. If a pituitary tumour is found,
the pituitary gland may be making too many hormones. This can cause other
problems in the body. Tumours that make hormones are called functioning tumours,
while those that do not make hormones are called non-functioning tumours.