|
Anal
Cancer Anal cancer, an uncommon
cancer, is a disease in which malignant cells are found in the anus. The anus is
the opening at the end of the rectum (the end part of the large intestine)
through which body waste passes. Cancer in the outer part of the anus is more
likely to occur in men; cancer of the inner part of the rectum (anal canal) is
more likely to occur in women. If your anus is often red, swollen, and sore, you
have a greater chance of getting anal cancer. Tumours found in the area of skin
with hair on it just outside the anus are skin tumours, not anal cancer.
 Like most cancers, anal cancer
is best treated when it is found early. You should see your doctor if you have
one or more of the following symptoms: bleeding from the rectum (even a small
amount), pain or pressure in the area around the anus, itching or discharge from
the anus, or a lump near the anus. Like most cancers, anal cancer
is best treated when it is found early. You should see your doctor if you have
one or more of the following symptoms: bleeding from the rectum (even a small
amount), pain or pressure in the area around the anus, itching or discharge from
the anus, or a lump near the anus.
If you have signs of cancer,
your doctor will usually examine the outside part of the anus and give you a
rectal examination. In a rectal examination, your doctor, wearing thin gloves,
puts a greased finger into the rectum and gently feels for lumps. Your doctor
may also check any material on the glove to see if there is blood in it. If you
feel pain when touched in the anal area, your doctor may give you medicine to
put you to sleep (general anaesthesia) in order to continue the examination.
Your doctor may cut out a small piece of tissue and look at it under a
microscope to see if there are any cancer cells. This procedure is called a
biopsy.
Your prognosis (chance of
recovery) and choice of treatment depend on the stage of your cancer (whether it
is just in the anus or has spread to other places in the body) and your general
state of health.
Stages Of Anal Cancer
Once anal cancer is found
(diagnosed), more tests will be done to find out if cancer cells have spread to
other parts of the body. This testing is called staging. To plan treatment, your
doctor needs to know the stage of your disease. The following stages are used
for anal cancer.
Stage 0 Or Carcinoma In Situ
Stage 0 anal cancer is very early cancer. The cancer is found only in the
top layer of anal tissue.

Stage I The cancer has
spread beyond the top layer of anal tissue and is smaller than 2 centimetres
(less than 1 inch).
Stage II Cancer has
spread beyond the top layer of anal tissue and is larger than 2 centimetres
(about 1 inch), but it has not spread to nearby organs or lymph nodes. (Lymph
nodes are small, bean-shaped structures found throughout the body. They produce
and store infection-fighting cells.)
Stage IIIA Cancer
has spread to the lymph nodes around the rectum or to nearby organs such as the
vagina or bladder.
Stage IIIB Cancer has
spread to the lymph nodes in the middle of the abdomen or in the groin, or the
cancer has spread to both nearby organs and the lymph nodes around the rectum.
Stage IV Cancer has
spread to distant lymph nodes within the abdomen or to organs in other parts of
the body.
Recurrent Recurrent
disease means that the cancer has come back (recurred) after it has been
treated. It may come back in the anus or in another part of the body.
How Anal Cancer Is
Treated
There are treatments for all
patients with anal cancer. Three kinds of treatment are used: surgery (taking
out the cancer in an operation) radiation therapy (using high-dose x-rays or
other high-energy rays to kill cancer cells) chemotherapy (using drugs to kill
cancer cells).
Surgery is a common way to
diagnose and treat anal cancer. Your doctor may take out the cancer using one of
the following methods:
Local resection is an operation
that takes out only the cancer. Often the ring of muscle around the anus that
opens and closes it (the sphincter muscle) can be saved during surgery so that
you will be able to pass your body wastes as before.
Abdominoperineal resection
 is
an operation in which the doctor removes the anus and the lower part of the
rectum by cutting into the abdomen and the perineum, which is the space between
the anus and the scrotum (in men) or the anus and the vulva (in women). Your
doctor will then make an opening (stoma) on the outside of the body for waste to
pass out of the body. This opening is called a colostomy. Although this
operation was once commonly used for anal cancer, it is not used as much today
because radiation therapy with or without chemotherapy is an equally effective
treatment option but does not require a colostomy. If you have a colostomy, you
will need to wear a special bag to collect body wastes. This bag, which sticks
to the skin around the stoma with a special glue, can be thrown away after it is
used. This bag does not show under clothing, and most is
an operation in which the doctor removes the anus and the lower part of the
rectum by cutting into the abdomen and the perineum, which is the space between
the anus and the scrotum (in men) or the anus and the vulva (in women). Your
doctor will then make an opening (stoma) on the outside of the body for waste to
pass out of the body. This opening is called a colostomy. Although this
operation was once commonly used for anal cancer, it is not used as much today
because radiation therapy with or without chemotherapy is an equally effective
treatment option but does not require a colostomy. If you have a colostomy, you
will need to wear a special bag to collect body wastes. This bag, which sticks
to the skin around the stoma with a special glue, can be thrown away after it is
used. This bag does not show under clothing, and most
 people
take care of these bags themselves. Lymph nodes may also be taken out at the
same time or in a separate operation (lymph node dissection). people
take care of these bags themselves. Lymph nodes may also be taken out at the
same time or in a separate operation (lymph node dissection).
Radiation therapy uses x-rays
or other high-energy rays to kill cancer cells and shrink tumours. Radiation may
come from a machine outside the body (external radiation therapy) or from
putting materials that produce radiation (radioisotopes) through thin plastic
tubes in the area where the cancer cells are found (internal radiation therapy).
Radiation can be used alone or in addition to other treatments.
Chemotherapy uses drugs to kill
cancer cells. Chemotherapy may be taken by pill, or it may be put into the body
by a needle in a vein or muscle. Chemotherapy is called a systemic treatment
because the drugs enter the bloodstream, travel through the body, and can kill
cancer cells throughout the body. Some chemotherapy drugs can also make cancer
cells more sensitive to radiation therapy. Radiation therapy and chemotherapy
can be used together to shrink tumours and make an abdominoperineal resection
unnecessary. When only limited surgery is required, the sphincter muscle can
often be saved.
STAGE 0 ANAL CANCER
Your treatment will probably be
local resection.
STAGE I ANAL CANCER
Your treatment may be one of
the following: 1. Local resection (for some small tumours). 2. External radiation
therapy with chemotherapy. Some patients may also receive internal radiation
therapy. 3. If cancer cells remain following therapy, you may need surgery of
the anal canal to remove the cancer.
STAGE II ANAL CANCER
Your treatment may be one of
the following: 1. Local resection (for small tumours). 2. External radiation
therapy with chemotherapy. Some patients may also receive internal radiation
therapy. 3. If cancer cells remain following therapy, you may need surgery of
the anal canal to remove the cancer.
STAGE IIIA ANAL CANCER
Your treatment may be one of
the following: 1. Radiation therapy with chemotherapy. 2. Surgery. Depending on
how much cancer remains following chemotherapy and radiation, local resection or
surgery to remove cancer in the anal canal may be done. 3. Clinical trials of
surgery (resection) followed by external radiation therapy. 4. Clinical trials
of surgery followed by chemotherapy if chemotherapy has not been used prior to
surgery.
STAGE IIIB ANAL CANCER
Your treatment will probably be
radiation therapy and chemotherapy followed by surgery. Depending on how much
cancer remains following chemotherapy and radiation, local resection or surgery
to remove the anus and the lower part of the rectum (abdominoperineal resection)
may be done. During surgery, the lymph nodes in the groin may be removed (lymph
node dissection).
STAGE IV ANAL CANCER
Your treatment may be one of
the following:
1. Surgery to relieve symptoms
2. Radiation therapy to relieve
symptoms
3. Chemotherapy and radiation
therapy to relieve symptoms
4. Clinical trials
BACK
|
|
Stomach
(Gastric) Cancer
Gastric cancer is a disease in which malignant
cells form in the lining of the stomach.
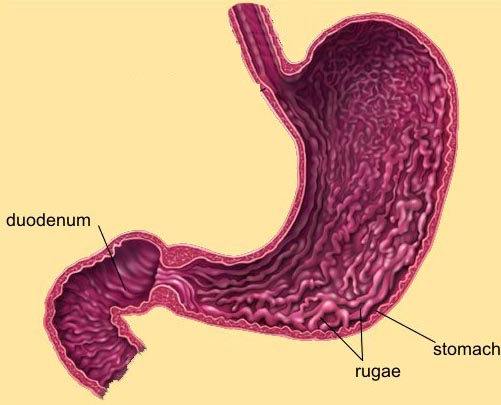 The
stomach is a J-shaped organ in the upper abdomen. It is part of the digestive
system, which processes nutrients (vitamins, minerals, carbohydrates, fats,
proteins, and water) in foods that are eaten and helps pass waste material out
of the body. Food moves from the throat to the stomach through a hollow,
muscular tube called the oesophagus. After leaving the stomach, partly-digested
food passes into the small intestine and then into the large intestine (the
colon). The
stomach is a J-shaped organ in the upper abdomen. It is part of the digestive
system, which processes nutrients (vitamins, minerals, carbohydrates, fats,
proteins, and water) in foods that are eaten and helps pass waste material out
of the body. Food moves from the throat to the stomach through a hollow,
muscular tube called the oesophagus. After leaving the stomach, partly-digested
food passes into the small intestine and then into the large intestine (the
colon).
The wall of the stomach is made up of 3 layers of tissue: the mucosal
(innermost) layer, the muscularis (middle) layer, and the serosal (outermost)
layer. Gastric cancer begins in the cells lining the mucosal layer and spreads
through the outer layers as it grows.
Stromal tumours of the stomach begin in supporting connective tissue and are
treated differently from gastric cancer.
Age, diet, and stomach disease can affect the risk of developing gastric cancer.
Risk factors include the following:
- Helicobacter pylori infection of the
stomach.
- Chronic gastritis (inflammation of the
stomach).
- Older age.
- Being male.
- A diet high in salted, smoked, or poorly
preserved foods and low in fruits and vegetables.
- Pernicious anaemia.
- Smoking cigarettes.
- Intestinal metaplasia.
- Familial adenomatous polyposis (FAP) or
gastric polyps.
- A mother, father, sister, or brother who
has had stomach cancer.
Possible signs of gastric cancer include
indigestion and stomach discomfort or pain. These and other symptoms may be caused by gastric cancer or by other conditions. In the early stages of gastric cancer, the following symptoms may occur:
- Indigestion and stomach
discomfort
- A bloated feeling after
eating
- Mild nausea
- Loss of appetite
- Heartburn
In more advanced stages of gastric cancer, the
following symptoms may occur:
- Blood in the stool
- Vomiting
- Weight loss
(unexplained)
- Stomach pain
- Jaundice (yellowing of
eyes and skin)
- Ascites (build-up of
fluid in the abdomen)
- Difficulty swallowing
A doctor should be consulted if any of these problems occur.
Tests that examine the stomach and oesophagus are used to detect (find) and
diagnose gastric cancer.
The following tests and procedures may be used: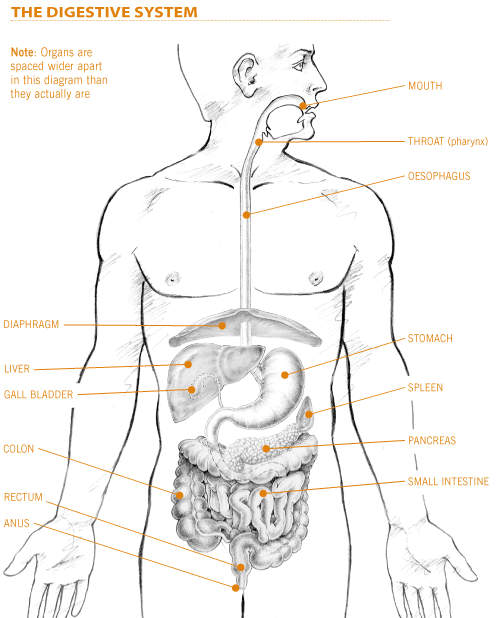
Physical exam and history: An exam of the body to check general signs of
health, including checking for signs of disease, such as lumps or anything else
that seems unusual. A history of the patientís health habits and past illnesses
and treatments will also be taken.
Blood chemistry studies: A procedure in
which a blood sample is checked to measure the amounts of certain substances
released into the blood by organs and tissues in the body. An unusual (higher or
lower than normal) amount of a substance can be a sign of disease in the organ
or tissue that produces it.
Complete blood count: A procedure in
which a sample of blood is drawn and checked for the following:
The number of red blood cells, white blood cells, and platelets.
The amount of haemoglobin (the protein that carries oxygen) in the red blood
cells.
The portion of the sample made up of red blood cells.
Upper endoscopy: A procedure to look
inside the oesophagus, stomach, and duodenum (first part of the small intestine)
to check for abnormal areas. An endoscope (a thin, lighted tube) is passed
through the mouth and down the throat into the oesophagus.
Faecal occult blood test: A test to
check stool (solid waste) for blood that can only be seen with a microscope.
Small samples of stool are placed on special cards and returned to the doctor or
laboratory for testing.
Barium swallow: A series of x-rays of
the oesophagus and stomach. The patient drinks a liquid that contains barium (a
silver-white metallic compound). The liquid coats the oesophagus and stomach and
x-rays are taken. This procedure is also called an upper GI series.
Biopsy: The removal of cells or tissues
so they can be viewed under a microscope to check for signs of cancer. A biopsy
of the stomach is usually done during the endoscopy.
CT scan (CAT scan): A procedure that
makes a series of detailed pictures of areas inside the body, taken from
different angles. The pictures are made by a computer linked to an x-ray
machine. A dye may be injected into a vein or swallowed to help the organs or
tissues show up more clearly. This procedure is also called computed tomography,
computerized tomography, or computerized axial tomography.
Certain factors affect treatment options and
prognosis (chance of recovery).
The treatment options and prognosis (chance of recovery) depend on the stage and
extent of the cancer (whether it is in the stomach only or has spread to lymph
nodes or other places in the body) and the patientís general health.
After gastric cancer has been diagnosed, tests are done to find out if cancer
cells have spread within the stomach or to other parts of the body.
The process used to find out if cancer has spread within the stomach or to other
parts of the body is called staging. The information gathered from the staging
process determines the stage of the disease. It is important to know the stage
in order to plan the best treatment.
The following tests and procedures may be used in the staging process:
ŖHCG (beta human chorionic gonadotropin), CA-125, and CEA (carcinoembryonic
antigen) assays: Tests that measure the levels of ŖHCG, CA-125, and CEA in
the blood. These substances are released into the bloodstream from both cancer
cells and normal cells. When found in higher than normal amounts, they can be a
sign of gastric cancer or other conditions.
Chest x-ray: An x-ray of the organs and
bones inside the chest. An x-ray is a type of energy beam that can go through
the body and onto film, making a picture of areas inside the body.
Endoscopic ultrasound (EUS): A
procedure in which an endoscope (a thin, lighted tube) is inserted into the
body. The endoscope is used to bounce high-energy sound waves (ultrasound) off
internal tissues or organs and make echoes. The echoes form a picture of body
tissues called a sonogram. This procedure is also called endosonography.
CT scan (CAT scan): A procedure that
makes a series of detailed pictures of areas inside the body, taken from
different angles. The pictures are made by a computer linked to an x-ray
machine. A dye may be injected into a vein or swallowed to help the organs or
tissues show up more clearly. This procedure is also called computed tomography,
computerized tomography, or computerized axial tomography.
Laparoscopy: A surgical procedure to
look at the organs inside the abdomen to check for abnormal areas. An incision
(cut) is made in the abdominal wall and a laparoscope (a thin, lighted tube) is
inserted into the abdomen. Tissue samples and lymph nodes may be removed for
biopsy.
PET scan (positron emission tomography
scan): A procedure to find malignant tumour cells in the body. A small
amount of radionuclide glucose (sugar) is injected into a vein. The PET scanner
rotates around the body and makes a picture of where glucose is being used in
the body. Malignant tumour cells show up brighter in the picture because they
are more active and take up more glucose than normal cells.
The following stages are used for gastric
cancer:
Stage 0 (Carcinoma in Situ)
In stage 0, cancer is found only in the inside lining of the mucosal (innermost)
layer of the stomach wall. Stage 0 is also called carcinoma in situ.
Stage I
Stage I gastric cancer is divided into stage IA and stage IB, depending on where
the cancer has spread.
Stage IA: Cancer has spread completely through the mucosal (innermost) layer of
the stomach wall.
Stage IB: Cancer has spread: completely through the mucosal (innermost) layer of
the stomach wall and is found in up to 6 lymph nodes near the tumour; or to the
muscularis (middle) layer of the stomach wall.
Stage II
In stage II gastric cancer, cancer has spread: completely through the mucosal
(innermost) layer of the stomach wall and is found in 7 to 15 lymph nodes near
the tumour; or to the muscularis (middle) layer of the stomach wall and is found
in up to 6 lymph nodes near the tumour; or to the serosal (outermost) layer of
the stomach wall but not to lymph nodes or other organs.
Stage III
Stage III gastric cancer is divided into stage IIIA and stage IIIB depending on
where the cancer has spread.
Stage IIIA: Cancer has spread to:
the muscularis (middle) layer of the stomach wall and is found in 7 to 15 lymph
nodes near the tumour; or the serosal (outermost) layer of the stomach wall and
is found in 1 to 6 lymph nodes near the tumour; or organs next to the stomach
but not to lymph nodes or other parts of the body.
Stage IIIB: Cancer has spread to the serosal (outermost) layer of the stomach
wall and is found in 7 to 15 lymph nodes near the tumour.
Stage IV
In stage IV, cancer has spread to: organs next to the stomach and to at least
one lymph node; or more than 15 lymph nodes; or other parts of the body.
There are different types of treatment for
patients with gastric cancer
Different types of treatments are
available for patients with
gastric
cancer. Some treatments are standard (the currently
used treatment), and some are being tested in
clinical trials. Before starting treatment, patients
may want to think about taking part in a clinical trial. A treatment clinical
trial is a research study meant to help improve current treatments or obtain
information on new treatments for patients with cancer. When clinical trials
show that a new treatment is better than the
"standard" treatment, the new treatment may become the
standard treatment.
Four types of standard treatment are used:
Surgery
Surgery is a common
treatment of all stages of gastric cancer. The following types of surgery may be
used:
- Subtotal
gastrectomy: Removal of the part of the
stomach that contains cancer, nearby
lymph nodes, and parts of other
tissues and
organs near the
tumour. The
spleen may be removed. The spleen is an organ in the
upper
abdomen that filters the blood and removes old blood
cells.
- Total gastrectomy:
Removal of the entire stomach, nearby lymph nodes, and parts of the
oesophagus,
small intestine, and other tissues near the tumour.
The spleen may be removed. The oesophagus is connected to the small intestine
so the patient can continue to eat and swallow.
If the tumour is blocking the opening to the
stomach but the cancer cannot be completely removed by standard surgery, the
following procedures may be used:
-
Endoluminal stent placement: A procedure to insert a
stent (a thin, expandable tube) in order to keep a
passage (such as arteries or the oesophagus) open. For tumours blocking the
opening to the stomach, surgery may be done to place a stent from the
oesophagus to the stomach to allow the patient to eat normally.
- Endoscopic laser surgery:
A procedure in which an
endoscope (a thin, lighted tube) with a
laser attached is inserted into the body. A laser is
an intense beam of light that can be used as a knife.
-
Electrocautery: A procedure that uses an electrical
current to create heat. This is sometimes used to remove
lesions or control bleeding.
Chemotherapy
Chemotherapy is a
cancer treatment that uses drugs to stop the growth of cancer
cells, either by killing the cells or by stopping the
cells from dividing. When chemotherapy is taken by mouth or
injected into a vein or muscle, the drugs enter the
bloodstream and can reach cancer cells throughout the body (systemic
chemotherapy). When chemotherapy is placed directly in
the spinal column, a body cavity such as the abdomen, or an organ, the drugs
mainly affect cancer cells in those areas. The way the chemotherapy is given
depends on the type and stage of the cancer being treated.
Radiation therapy
Radiation therapy
is a cancer treatment that uses high-energy
x-rays or other types of
radiation to kill cancer cells. There are two types of
radiation therapy.
External radiation therapy uses a machine outside the
body to send radiation toward the cancer.
Internal radiation therapy uses a
radioactive substance sealed in needles,
seeds, wires, or
catheters that are placed directly into or near the
cancer. The way the radiation therapy is given depends on the type and stage of
the cancer being treated.
Chemoradiation
Chemoradiation combines chemotherapy and radiation therapy to increase the
effects of both. Chemoradiation treatment given after surgery to increase the
chances of a cure is called
adjuvant therapy. If it is given before surgery, it is
called
neoadjuvant therapy.
Other types of
treatment are being tested in clinical trials. These include the following:
Biologic therapy
Biologic therapy
is a treatment that uses the patientís
immune system to fight cancer. Substances made by the
body or made in a laboratory are used to boost, direct, or restore the bodyís
natural defences against cancer. This type of cancer treatment is also called
biotherapy or immunotherapy.
Treatment Options by Stage
Stage 0 Gastric Cancer (Carcinoma in Situ)
Treatment of stage 0 gastric cancer may include the following:
Surgery (total or subtotal gastrectomy).
Stage I and Stage II Gastric Cancer
Treatment of stage I and stage II gastric cancer may include the following:
Surgery (total or subtotal gastrectomy).
Surgery (total or subtotal gastrectomy) followed by chemoradiation therapy.
A clinical trial of chemoradiation therapy given before surgery.
Stage III Gastric Cancer
Treatment of stage III gastric cancer may include the following:
Surgery (total gastrectomy).
Surgery followed by chemoradiation therapy.
A clinical trial of chemoradiation therapy given before surgery.
Stage IV Gastric Cancer
Treatment of stage IV gastric cancer that has not spread to distant organs may
include the following:
Surgery (total gastrectomy) followed by chemoradiation therapy.
A clinical trial of chemoradiation therapy given before surgery.
Treatment of stage IV gastric cancer that has spread to distant organs may
include the following:
Chemotherapy as palliative therapy to relieve symptoms and improve the quality
of life.
Endoscopic laser surgery or endoluminal stent placement as palliative therapy to
relieve symptoms and improve the quality of life.
Radiation therapy as palliative therapy to stop bleeding, relieve pain, or
shrink a tumour that is blocking the opening to the stomach.
Surgery as palliative therapy to stop bleeding or shrink a tumour that is
blocking the opening to the stomach.
Treatment Options for Recurrent Gastric Cancer
Treatment of recurrent gastric cancer may include the following:
Chemotherapy as palliative therapy to relieve symptoms and improve the quality
of life.
Endoscopic laser surgery or electrocautery as palliative therapy to relieve
symptoms and improve the quality of life.
Radiation therapy as palliative therapy to stop bleeding, relieve pain, or
shrink a tumour that is blocking the stomach.
A clinical trial of new anticancer drugs or biologic therapy.
BACK
|
Small
Intestine Cancer
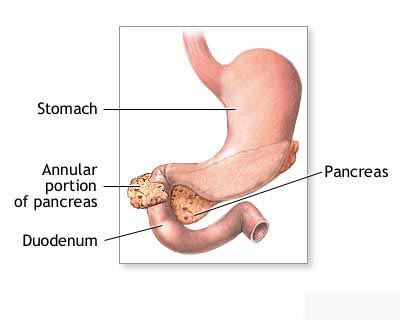
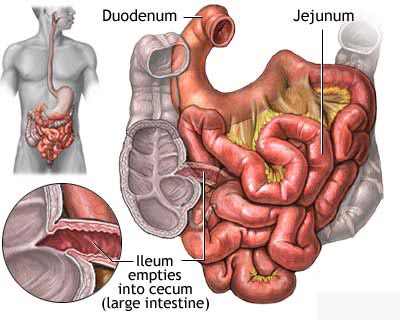
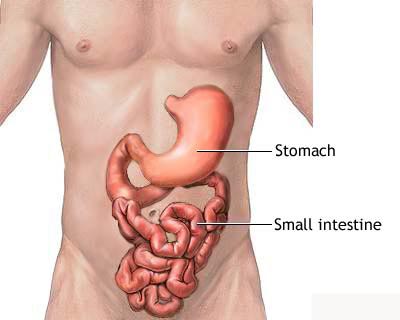 The
small intestine is the portion of the digestive system most responsible for
absorption of nutrients from food into the bloodstream. The pyloric sphincter
governs the passage of partly digested food from the stomach into the duodenum.
This short first portion of the small intestine is followed by the jejunum and
the ileum. The ileocecal valve of the ileum passes digested material into the
large intestine The
small intestine is the portion of the digestive system most responsible for
absorption of nutrients from food into the bloodstream. The pyloric sphincter
governs the passage of partly digested food from the stomach into the duodenum.
This short first portion of the small intestine is followed by the jejunum and
the ileum. The ileocecal valve of the ileum passes digested material into the
large intestineCancer of the small intestine, a rare cancer,
is a disease in which cancer cells are found in the tissues of the small
intestine. The small intestine is a long tube that folds many times to fit
inside the abdomen. It connects the stomach to the large intestine (bowel). In
the small intestine, food is broken down to remove vitamins, minerals, proteins,
carbohydrates, and fats.
A doctor should be seen if there are any of
the following:
- Pain or cramps in the middle of
the abdomen.
- Weight loss without dieting.
- A lump in the abdomen.
- Blood in the stool.
If there are symptoms, a doctor will usually
order an upper gastrointestinal x-ray (also called an upper GI series). For this
examination, a patient drinks a liquid containing barium, which makes the
stomach and intestine easier to see in the x-ray. This test is usually performed
in a doctorís office or in a hospital radiology department.
The doctor may also do a CT scan, a special
x-ray that uses a computer to make a picture of the inside of the abdomen. An
ultrasound, which uses sound waves to find tumours, or an MRI scan, which uses
magnetic waves to make a picture of the abdomen, may also be done.
The doctor may put a thin lighted tube called
an endoscope down the throat, through the stomach, and into the first part of
the small intestine. The doctor may cut out a small piece of tissue during the
endoscopy. This is called a biopsy. The tissue is then looked at under a
microscope to see if it contains cancer cells.
The chance of recovery (prognosis) depends on
the type of cancer, whether it is just in the small intestine or has spread to
other tissues, and the patientís overall health.
Stages of cancer of the small intestine
Once small intestine cancer is found, more tests will be done to find out if
cancer cells have spread to other parts of the body. Although there is a staging
system for cancer of the small intestine, for treatment purposes this cancer is
grouped based on what kind of cells are found. The types of cancer found in the
small intestine include adenocarcinoma, sarcoma, and carcinoid tumours.
Adenocarcinoma
Adenocarcinoma starts in the lining of the small intestine and is the most
common type of cancer of the small intestine. These tumours occur most often in
the part of the small intestine nearest the stomach. These cancers often grow
and block the bowel.
Leiomyosarcoma
Leiomyosarcomas are cancers that start growing in the smooth muscle lining of
the small intestine.
Recurrent
Recurrent disease means that the cancer has come back (recurred) after it has
been treated. It may come back in the small intestine or in another part of the
body.
How cancer of the small intestine is
treated
There are treatments for all patients with
cancer of the small intestine. Three kinds of treatment are used:
- Surgery (taking out the
cancer).
- Radiation therapy (using
high-dose x-rays to kill cancer cells).
- Chemotherapy (using drugs to
kill cancer cells).
Surgery to remove the cancer is the most
common treatment. Lymph nodes in the area may also be removed and looked at
under a microscope to see if they contain cancer. If the tumour is large, a
doctor may cut out a section of the small intestine containing the cancer and
reconnect the intestine.
Radiation therapy uses high-energy x-rays to
kill cancer cells and shrink tumours. Radiation may come from a machine outside
the body (external radiation therapy) or from putting materials that produce
radiation (radioisotopes) through thin plastic tubes in the area where the
cancer cells are found (internal radiation therapy). Drugs that make the cancer
cells more sensitive to radiation (radio sensitizers) are sometimes given along
with radiation. Radiation can be used alone or in addition to surgery and/or
chemotherapy.
Chemotherapy uses drugs to kill cancer cells.
Chemotherapy may be taken by pill, or it may be put in the body through a needle
in a vein or muscle. Chemotherapy is called a systemic treatment because the
drug enters the bloodstream, travels through the body, and can kill cancer cells
outside the intestine.
If the doctor removes all the cancer that can
be seen at the time of the operation, the patient may be given chemotherapy
after surgery to kill any cancer cells that are left. Chemotherapy given after
an operation is called adjuvant chemotherapy.
Biological therapy (using the bodyís immune
system to fight cancer) is being studied in clinical trials. Biological therapy
tries to get the body to fight cancer. It uses materials made by the body or
made in a laboratory to boost, direct, or restore the bodyís natural defences
against disease. Biological therapy is sometimes called biological response
modifier (BRM) therapy or immunotherapy.
Small Intestine Adenocarcinoma
Treatment may be one of the following:
- Surgery to cut out the tumour.
- Surgery to allow food in the
small intestine to go around the cancer (bypass) if the cancer cannot be
removed.
- Radiation therapy to relieve
symptoms.
- A clinical trial of radiation
plus drugs to make cancer cells more sensitive to radiation (radio
sensitizers), with or without chemotherapy.
- A clinical trial of
chemotherapy or biological therapy.
Small Intestine Leiomyosarcoma
Treatment may be one of the following:
- Surgery to remove the cancer.
- Surgery to allow food in the
small intestine to go around the cancer (bypass) if the cancer cannot be
removed.
- Radiation therapy.
- Surgery, chemotherapy, or
radiation therapy to relieve symptoms.
- A clinical trial of
chemotherapy or biological therapy.
Recurrent Small Intestine Cancer
If the cancer comes back in another part of
the body, treatment will probably be a clinical trial of chemotherapy or
biological therapy.
If the cancer has come back only in one area,
treatment may be one of the following:
- Surgery to remove the cancer.
- Radiation therapy or
chemotherapy to relieve symptoms.
- A clinical trial of radiation
with drugs to make the cancer cells more sensitive to radiation (radio
sensitizers), with or without chemotherapy.
BACK
|
|
Bile Duct Cancer
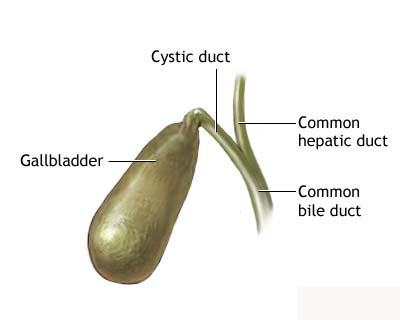
Extrahepatic bile duct cancer,
a rare cancer, is a disease in which malignant cells are found in the tissues of
the extrahepatic bile duct. The bile duct is a tube that connects the liver and
the gallbladder to the small intestine. The part of the bile duct that is
outside the liver is called the extrahepatic bile duct. A fluid called bile,
which is made by the liver and breaks down fats during digestion, is stored in
the gallbladder. When food is being broken down in the intestines, bile is
released from the gallbladder through the bile duct to the first part of the
small intestine.
A doctor should be seen if
there are any of the following symptoms:
 Yellowing of the
skin (jaundice) Yellowing of the
skin (jaundice)
Pain in the
abdomen
Fever
Itching
If there are symptoms, a doctor
will perform an examination and order tests to see if there is cancer. A patient
may have an ultrasound, a test that uses sound waves to find tumours. A patient
may also have a CT (computed tomographic) scan, which is a special type of x-ray
that uses a computer to make a picture of the inside of the abdomen. Another
special scan called magnetic resonance imaging (MRI), which uses magnetic waves
to make a picture of the inside of the abdomen, may be done as well.
A doctor may perform a test
called an ERCP (endoscopic retrograde cholangiopancreatography). During this
test, a flexible tube is put down the throat, through the stomach, and into the
small intestine. The doctor can see through the tube and inject dye into the
drainage tube (duct) of the pancreas so that the area can be seen more clearly
on an x-ray.
PTC (percutaneous transhepatic
cholangiography) is another test that can help find cancer of the extrahepatic
bile duct. During this test, a thin needle is put into the liver through the
right side of the patient. Dye is injected through the needle into the bile duct
in the liver so that blockages can be seen on x-rays.
If tissue that is not normal is
found, the doctor may remove a small amount of fluid or tissue from the bile
duct and look at it under the microscope to see if there are any cancer cells.
This procedure is called a biopsy and is usually done during the PTC or ERCP.
Because it is sometimes hard to
tell whether a patient has cancer or another disease, surgery may be needed to
see if there is cancer of the bile duct. If this is the case, the doctor will
cut into the abdomen and look at the bile duct and the tissues around it for
cancer. If there is cancer and if it looks like it has not spread to other
tissues, the doctor may remove the cancer or relieve blockages caused by the
tumour.
The chance of recovery
(prognosis) and choice of treatment depends on the location of the cancer in the
bile duct, the stage of the cancer (whether it is only in the bile duct or has
spread to other places), and the patientís general health.
Stages of extrahepatic bile
duct cancer
Once extrahepatic bile duct
cancer is found (diagnosed), more tests will be done to find out if cancer cells
have spread to other parts of the body. This is called staging. To plan
treatment, a doctor needs to know the stage of the cancer. The following stages
are used for extrahepatic bile duct cancer:
Localized
The cancer is only in the area
where it began and can be removed in an operation.
Unresectable
All of the cancer cannot be
removed in an operation. The cancer may have spread to nearby organs and lymph
nodes or to other parts of the body. (Lymph nodes are small bean-shaped
structures that are found throughout the body. They produce and store
infection-fighting cells.)
Recurrent
Recurrent disease means that
the cancer has come back (recurred) after it has been treated. It may come back
in the bile duct or in another part of the body.
How extrahepatic bile duct
cancer is treated
There are treatments for all
patients with extrahepatic bile duct cancer. Two kinds of treatment are used:
- Surgery (taking
out the cancer or taking steps to relieve symptoms caused by the cancer)
- Radiation
therapy (using high-dose x-rays to kill cancer cells)
Other treatments for
extrahepatic bile duct cancer are being studied in clinical trials. These
include:
- Chemotherapy
(using drugs to kill cancer cells)
- Biological
therapy (using the bodyís immune system to fight cancer)
Surgery is a common treatment
of extrahepatic bile duct cancer. If the cancer is small and is only in the bile
duct, a doctor may remove the whole bile duct and make a new duct by connecting
the duct openings in the liver to the intestine. The doctor will also remove
lymph nodes and look at them under the microscope to see if they contain cancer.
If the cancer has spread outside the bile duct, a surgeon may remove the bile
duct and the tissues around it.
If the cancer has spread and it
cannot be removed, the doctor may do surgery to relieve symptoms. If the cancer
is blocking the small intestine and bile builds up in the gallbladder, the
doctor may do surgery to go around (bypass) all or part of the small intestine.
During this operation, the doctor will cut the gallbladder or bile duct and sew
it to the small intestine. This is called biliary bypass. Surgery or x-ray
procedures may also be done to put in a tube (catheter) to drain bile that has
built up in the area. During these procedures, the doctor may make the catheter
drain through a tube to the outside of the body or the catheter may go around
the blocked area and drain the bile to the small intestine. In addition, if the
cancer is blocking the flow of food from the stomach, the stomach may be sewn
directly to the small intestine so the patient can continue to eat normally.
Radiation therapy is the use of
high-energy x-rays to kill cancer cells and shrink tumours. Radiation may come
from a machine outside the body (external-beam radiation therapy) or from
putting materials that produce radiation (radioisotopes) through thin plastic
tubes into the area where the cancer cells are found (internal radiation
therapy).
Chemotherapy is the use of
drugs to kill cancer cells. Chemotherapy may be taken by pill, or it may be put
into the body by inserting a needle into a vein or muscle. Chemotherapy is
called a systemic treatment because the drug enters the bloodstream, travels
through the body, and can kill cancer cells outside the bile duct.
Biological therapy tries to get
the body to fight cancer. It uses materials made by the body or made in a
laboratory to boost, direct, or restore the bodyís natural defences against
disease. Biological therapy is sometimes called biological response modifier (BRM)
therapy or immunotherapy. This treatment is currently only being given in
clinical trials.
Localized
Extrahepatic Bile Duct Cancer
Treatment may be one of the
following:
- Surgery to
remove the cancer.
- Surgery to
remove the cancer followed by external-beam radiation therapy.
Unresectable
Extrahepatic Bile Duct Cancer
Treatment may be one of the
following:
- Surgery or other
procedures to bypass blockage in the bile duct.
- Surgery or other
procedures to bypass blockage in the bile duct followed by external-beam
radiation therapy or internal radiation therapy.
- Clinical trials
of radiation therapy with drugs to make the cancer cells more sensitive to
radiation (radiosensitizers).
- Clinical trials
of chemotherapy or biological therapy.
Recurrent
Extrahepatic Bile Duct Cancer
Treatment depends on many
factors, including where the cancer came back and what treatment the patient
received before. Clinical trials are testing new treatments.
BACK
|
|
Gastrointestinal Cancer
Gastrointestinal carcinoid
tumours are cancers in which malignant cells are found in certain hormone-making
cells of the digestive, or gastrointestinal, system. The digestive system
absorbs vitamins, minerals, carbohydrates, fats, proteins, and water from the
food that is eaten and stores waste until the body eliminates it. The digestive
system is made up of the stomach and the small and large intestines. The last 6
feet of intestine is called the colon. The last 10 inches of the colon is the
rectum. The appendix is an organ attached to the large intestine.
There are often no signs of a
gastrointestinal carcinoid tumour in its early stages. Often the cancer will
make too much of some of the hormones, which can cause symptoms. A doctor should
be seen if the following symptoms persist:
- Pain in the
abdomen.
- Flushing and
swelling of the skin of the face and neck.
- Wheezing.
- Diarrhoea.
- Symptoms of
heart failure, including breathlessness.
If there are symptoms, a doctor
may order blood and urine tests to look for signs of cancer. Other tests may
also be done. If there is a carcinoid tumour, the patient has a greater chance
of getting other cancers in the digestive system, either at the same time or at
a later time.
The chance of recovery
(prognosis) and choice of treatment depend on whether the cancer is just in the
gastrointestinal system or has spread to other places, and on the patient's
general state of health.
There are treatments for all
patients with gastrointestinal carcinoid tumours. Four kinds of treatment are
used:
- Surgery (taking
out the cancer).
- Radiation
therapy (using high-dose x-rays to kill cancer cells).
- Biological
therapy (using the body's natural immune system to fight cancer).
- Chemotherapy
(using drugs to kill cancer cells).
Depending on where the cancer
started, the doctor may take out the cancer using one of the following
operations:
- A simple
appendectomy removes the appendix. If part of the colon is also taken out, the
operation is called a hemicolectomy. The doctor may also remove lymph nodes
and look at them under a microscope to see if they contain cancer.
- Local excision
uses a special instrument inserted into the colon or rectum through the anus
to cut the tumour out. This operation can be used for very small tumours.
- Fulguration uses
a special tool inserted into the colon or rectum through the anus. An electric
current is then used to burn the tumour away.
- Bowel resection
takes out the cancer and a small amount of healthy tissue on either side. The
healthy parts of the bowel are then sewn together. The doctor will also remove
lymph nodes and have them looked at under a microscope to see if they contain
cancer.
- Cryosurgery
kills the cancer by freezing it.
- Hepatic artery
ligation cuts and ties off the main blood vessel that brings blood into the
liver (the hepatic artery).
- Hepatic artery
embolization uses drugs or other agents to reduce or block the flow of blood
to the liver in order to kill cancer cells growing in the liver.
Radiation therapy uses
high-energy x-rays to kill cancer cells and shrink tumours. Radiation may come
from a machine outside the body (external radiation therapy) or from putting
materials that produce radiation (radioisotopes) through thin plastic tubes in
the area where the cancer cells are found (internal radiation therapy).
Chemotherapy uses drugs to kill
cancer cells. Chemotherapy may be taken by pill, or it may be put into the body
by a needle in the vein or muscle. Chemotherapy is called a systemic treatment
because the drug enters the bloodstream, travels through the body, and can kill
cancer cells outside the digestive system.
Biological therapy tries to get
the patient's body to fight the cancer. It uses materials made by the body or
made in a laboratory to boost, direct, or restore the body's natural defences
against disease. Biological therapy is sometimes called biological response
modifier (BRM) therapy or immunotherapy.
Treatment by type
Treatment of gastrointestinal
carcinoid tumour depends on the type of tumour, the stage, and the patient's
overall health.
Standard treatment may be
considered because of its effectiveness in patients in past studies, or
participation in a clinical trial may be considered. Not all patients are cured
with standard therapy and some standard treatments may have more side effects
than are desired. For these reasons, clinical trials are designed to find better
ways to treat cancer patients and are based on the most up-to-date information.
Localized
Gastrointestinal Carcinoid tumours
If the cancer started in the
appendix, the treatment will probably be surgery to remove the appendix
(appendectomy) with or without removal of part of the colon (hemicolectomy) and
lymph nodes.
If the cancer started in the
rectum, treatment will probably be simple surgery to remove the cancer, surgery
using electric current to burn the cancer away, surgery to remove part of the
rectum, or surgery to remove the anus and part of the rectum. An opening will be
made for waste to pass out of the body (colostomy) into a disposable bag
attached near the colostomy (colostomy bag).
If the cancer started in the
small intestine, the treatment will probably be surgery to remove part of the
bowel (bowel resection). Lymph nodes may also be taken out and looked at under
the microscope to see if they contain cancer.
If the cancer started in the
stomach, pancreas, or colon, the treatment will probably be surgery to remove
the organ affected by the cancer and possibly other nearby organs.
Regional
Gastrointestinal Carcinoid tumours
The treatment will probably be
surgery to remove the organ affected by the cancer and possibly other nearby
organs.
Metastatic
Gastrointestinal Carcinoid tumours
Treatment may be one of the
following:
- Surgery to
relieve symptoms caused by the cancer. Surgery to freeze and kill the cancer
may also be performed.
- Chemotherapy to
relieve symptoms caused by the cancer.
- Chemotherapy
injected directly into the hepatic artery to block the artery and kill cancer
cells growing in the liver.
- Radiation
therapy to relieve symptoms caused by the cancer.
- Radioactive
substances injected into the cancer to relieve the symptoms caused by the
cancer.
- Biological or
immunological therapy.
Carcinoid syndrome
Treatment options for
metastatic carcinoid tumour may be one of the following:
- Surgery to
remove the cancer.
- Surgery to cut
and tie the main artery that goes to the liver (hepatic artery ligation) or
injecting chemotherapy into the liver through the hepatic artery to block the
artery and kill cancer cells growing in the liver.
- Drugs designed
to relieve symptoms caused by the cancer.
- Biological
therapy to relieve symptoms caused by the cancer.
- A clinical trial
of new combinations of chemotherapy drugs.
BACK
|
|
Colon
Cancer
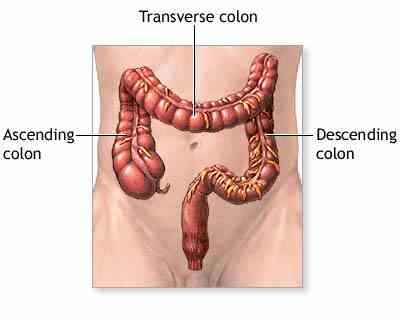
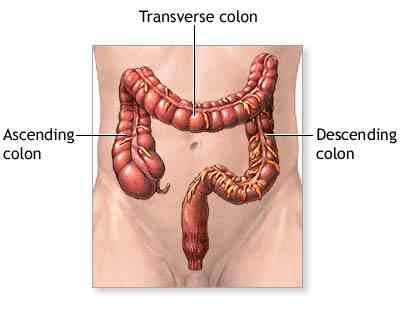
The colon is part of a section
of the digestive tract called the large intestine. The large intestine is a tube
that is 5 to 6 feet in length. The first 5 feet make up the colon, which
connects to about 6 inches of rectum, and ends with the anus. By the time food
reaches the colon (about 3 to 8 hours after eating), the nutrients have been
absorbed and it has become a liquid waste product. The colon's function is to
change this liquid waste into stool. The stool can spend anywhere from 10 hours
to several days in the colon. It has been suggested that the longer stool
remains in the colon, the higher the risk for colon cancer, but this has not
been proven.
What is colon cancer?
Colon cancer is malignant
tissue that grows in the wall of the colon. The majority of tumours begin when
normal tissue in the colon wall forms an adenomatous polyp, or pre-cancerous
growth projecting from the colon wall. As this polyp grows larger, the tumour is
formed. This process can take many years, which allows time for early detection
with screening tests.
Some tumours and polyps may
bleed intermittently, and this blood can be detected in stool samples by a test
called faecal occult blood testing (FOBT). By itself, FOBT only finds about 24%
of cancers. The sigmoidoscope is a slender, flexible tube that has the ability to view about ᄑ
of the colon. If a polyp or tumour is detected with this test, the patient must
be referred for a full colonoscopy.
The colonoscope is
similar to the sigmoidoscope, but is longer, and can view the entire colon. If a
polyp is found, the physician can remove it, and send it to a pathology lab to
determine if it is adenomatous (cancerous). As a screening method, the American
Cancer Society recommends that a colonoscopy be done every 10 years after age
50. Patients with a family or personal history should have more frequent
screenings, beginning at an earlier age than their relative was diagnosed.
Patients with a history of ulcerative colitis are also at increased risk and
should have more frequent screening than the general public. Patients should
talk with their doctor about which screening method is best for them, and how
often it should be performed.
What are the Signs of Colon
Cancer? 
Unfortunately, the early stages
of colon cancer may not have any symptoms. This is why it is important to have
screening tests done even though you feel well. As the polyp grows into a
tumour, it may bleed or obstruct the colon, causing symptoms. These symptoms
include:
- Bleeding from the rectum
- Blood in the stool or toilet
after a bowel movement
- A change in the shape of the
stool (i.e. thinning)
- Cramping pain in the abdomen
- Feeling the need to have a
bowel movement when you don't have to have one
As you can see, these symptoms
can also be caused by other conditions. If you experience these symptoms, you
should be checked by a doctor.
How is Colon Cancer Diagnosed
and Staged?
After a cancer has been found,
the stage must be determined to decide on appropriate treatment. The stage tells
how far the tumour has invaded the colon wall, and if it has spread to other
parts of the body.
- Stage 0 (also called
carcinoma in situ) - the cancer is confined to the outermost portion of the
colon wall.
- Stage I - the cancer has
spread to the second and third layer of the colon wall, but not to the outer
colon wall or beyond. This is also called Dukes' A colon cancer.
- Stage II - the cancer has
spread through the colon wall, but has not invaded any lymph nodes (these are
small structures that help in fighting infection and disease). This is also
called Dukes' B colon cancer.
- Stage III - the cancer has
spread through the colon wall and into lymph nodes, but has not spread to
other areas of the body. This is also called Dukes' C colon cancer.
- Stage IV - the cancer has
spread to other areas of the body (i.e. liver and lungs). This is also called
Dukes' D colon cancer.
After the tumour and lymph
nodes are removed by a surgeon, they are examined by a pathologist, who
determines how much of the colon wall and lymph nodes have been invaded by
tumour. Patients with invasive cancer (stages II, III, and IV) require a staging
workup, including full colonoscopy, carcinoembryonic antigen (CEA) level (a
marker for colon cancer found in the blood), chest x-ray, and CT scan of the
abdomen and pelvis, to determine if the cancer has spread.
What are the Treatments for
Colon Cancer?
 Surgery Surgery
Surgery is the most common
treatment for colon cancer. If the cancer is limited to a polyp, the patient can
undergo a polypectomy (removal of the polyp), or a local excision, where a small
amount of surrounding tissue is also removed. If the tumour invades the bowel
wall or surrounding tissues, the patient will require a partial resection
(removal of the cancer and a portion of the bowel) and removal of local lymph
nodes to determine if the cancer has spread into them. After the tumour is
removed, the two ends of the remaining colon are reconnected, allowing normal
bowel function. In some situations, it may not be possible to reconnect the
colon, and a colostomy (an opening in the abdominal wall to allow passage of
stool) is needed.
Chemotherapy
Despite the fact that a
majority of patients have the entire tumour removed by surgery, as many as 40%
will develop a recurrence. Chemotherapy is given to reduce this chance of
recurrence. There is some controversy over patients with stage II disease
receiving chemotherapy. Studies have not consistently shown a benefit in
treating these patients. Generally, patients with stage II disease who present
with a bowel perforation or obstruction, or have poorly differentiated tumours
(determined by a pathologist), are considered at higher risk for recurrence, and
are treated with 6 to 8 months of Fluorouracil (5-FU) and Leucovorin (LV) (both
chemotherapy agents). Other patients with stage II disease are followed closely,
but generally receive no chemotherapy. Patients who present with stage III colon
cancer are typically treated with a regimen of
Fluorouracil and Leucovorin for 12 months.
Forty to fifty percent of
patients have metastatic (disease that has spread to other organs) at the time
of diagnosis, or have a recurrence of the disease after therapy. Unfortunately,
the prognosis for these patients is poor. The standard therapy for patients with
advanced disease is
Fluorouracil, Leucovorin, and
irinotecan (CPT-11). This regimen was found to be more
effective than Fluorouracil and Leucovorin alone in these patients. With this
therapy, an average of 39% of patients have a response, but the average survival
is still only 15 months. Patients and their physicians must weigh the benefits
of therapy versus the side effects of the treatment. Younger patients and those
in better physical shape are better able to tolerate therapy.
Two new medications,
capecitabine (Xeloda) and oxaliplatin, are also being used in the treatment of
advanced colon cancer. Capecitabine is currently approved by the FDA for the
treatment of advanced colon cancer that has failed treatment, but is still being
investigated in untreated patients. Oxaliplatin is widely used in Europe, but
has not yet been approved by the FDA for use in the United States. Currently,
patients can only receive this medication in a clinical trial.
Radiotherapy
Colon cancer is not typically
treated with radiation therapy. If the cancer has invaded another organ, or
adhered to the abdominal wall, radiation therapy may be one option. One way to
understand this is that radiation needs a "target". If the tumour has been
surgically resected, there is no target to radiate. If the tumour has spread to
other organs, chemotherapy is needed to reach all the tumour cells, whereas
radiation can only treat a small area.
BACK
|
|
Oesophageal
Cancer Oesophageal cancer is a disease in which
malignant cells form in the tissues of the oesophagus.
The oesophagus is the hollow, muscular tube that moves food and liquid from the
throat to the stomach. The wall of the oesophagus is made up of several layers
of tissue, including mucous membrane, muscle, and connective tissue. Oesophageal
cancer starts at the inside lining of the oesophagus and spreads outward through
the other layers as it grows.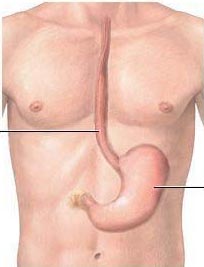 The two most common forms of oesophageal cancer are named for the type of cells
that become malignant (cancerous):
The two most common forms of oesophageal cancer are named for the type of cells
that become malignant (cancerous):
- Squamous cell carcinoma: Cancer that forms in squamous cells, the thin, flat
cells lining the oesophagus. This cancer is most often found in the upper and
middle part of the oesophagus, but can occur anywhere along the oesophagus. This
is also called epidermoid carcinoma.
- Adenocarcinoma: Cancer that begins in glandular (secretory) cells. Glandular
cells in the lining of the oesophagus produce and release fluids such as mucus.
Adenocarcinomas usually form in the lower part of the oesophagus, near the
stomach.
Smoking, heavy alcohol use, and Barrettís oesophagus can affect the risk of
developing oesophageal cancer.
Risk factors include the following:
- Tobacco use
- Heavy alcohol use
- Barrettís oesophagus: A condition in which the cells lining the lower part of
the oesophagus have changed or been replaced with abnormal cells that could lead
to cancer of the oesophagus. Gastric reflux (the backing up of stomach contents
into the lower section of the oesophagus) may irritate the oesophagus and, over
time, cause Barrettís oesophagus
- Older age
- Being male
- Being African-American
The most common signs of oesophageal cancer
are painful or difficult swallowing and weight loss.
These and other symptoms may be caused by oesophageal cancer or by other
conditions. A doctor should be consulted if any of the following problems occur
-
Painful or
difficult swallowing
-
Weight loss
-
Pain behind
the breastbone
-
Hoarseness
and cough
-
Indigestion and heartburn
Tests that examine the oesophagus are used to detect (find) and diagnose
oesophageal cancer. The following tests and procedures may be used:
Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a
type of energy beam that can go through the body and onto film, making a picture
of areas inside the body.
Barium swallow: A series of x-rays of the oesophagus and stomach. The patient
drinks a l iquid
that contains barium (a silver-white metallic compound). The liquid coats the
oesophagus and x-rays are taken. This procedure is also called an upper GI
series. iquid
that contains barium (a silver-white metallic compound). The liquid coats the
oesophagus and x-rays are taken. This procedure is also called an upper GI
series.
Oesophagoscopy: A procedure to look inside the oesophagus to check for abnormal
areas. An oesophagoscope (a thin, lighted tube) is inserted through the mouth
and down the throat into the oesophagus. Tissue samples may be taken for biopsy.
Biopsy: The removal of cells or tissues so they can be viewed under a microscope
to check for signs of cancer. The biopsy is usually done during an
oesophagoscopy. Sometimes a biopsy shows changes in the oesophagus that are not
cancer but may lead to cancer.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) and treatment options depend on the
following:
- The stage of the cancer
(whether it affects part of the oesophagus, involves the whole
oesophagus, or has spread to other places in the body)
- The size of the tumour
- The patientís general
health
- When oesophageal cancer is found very early, there is a better chance of
recovery. Oesophageal cancer is often in an advanced stage when it is diagnosed.
At later stages, oesophageal cancer can be treated but rarely can be cured.
Taking part in one of the clinical trials being done to improve treatment should
be considered.
 Stages
of Oesophageal Cancer Stages
of Oesophageal Cancer
After oesophageal cancer has been diagnosed, tests are done to find out if
cancer cells have spread within the oesophagus or to other parts of the body.
The following stages are used for oesophageal cancer:
Stage 0 (Carcinoma in Situ)
Stage I
Stage II
Stage III
Stage IV
After oesophageal cancer has been diagnosed, tests are done to find out if
cancer cells have spread within the oesophagus or to other parts of the body.
The process used to find out if cancer cells have spread within the oesophagus
or to other parts of the body is called staging. The information gathered from
the staging process determines the stage of the disease. It is important to know
the stage in order to plan treatment. The following tests and procedures may be
used in the staging process:
Bronchoscopy: A procedure to look inside the trachea and large airways in
the lung for abnormal areas. A bronchoscope (a thin, lighted tube) is inserted
through the nose or mouth into the trachea and lungs. Tissue samples may be
taken for biopsy.
Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a
type of energy beam that can go through the body and onto film, making a picture
of areas inside the body.
Laryngoscopy: A procedure in which the doctor examines the larynx (voice
box) with a mirror or with a laryngoscope (a thin, lighted tube).
CT scan (CAT scan): A procedure that makes a series of detailed pictures of
areas inside the body, taken from different angles. The pictures are made by a
computer linked to an x-ray machine. A dye may be injected into a vein or
swallowed to help the organs or tissues show up more clearly. This test is also
called computed tomography, computerized tomography, or computerized axial
tomography.
Endoscopic ultrasound (EUS): A procedure in which an endoscope (a thin,
lighted tube) is inserted into the body. The endoscope is used to bounce
high-energy sound waves (ultrasound) off internal tissues or organs and make
echoes. The echoes form a picture of body tissues called a sonogram. This
procedure is also called endosonography.
Thoracoscopy: A surgical procedure to look at the organs inside the chest
to check for abnormal areas. An incision (cut) is made between two ribs and a
thoracoscope (a thin, lighted tube) is inserted into the chest. Tissue samples
and lymph nodes may be removed for biopsy. In some cases, this procedure may be
used to remove portions of the oesophagus or lung.
Laparoscopy: A surgical procedure to look at the organs inside the
abdomen to check for abnormal areas. An incision (cut) is made in the abdominal
wall and a laparoscope (a thin, lighted tube) is inserted into the abdomen.
Tissue samples and lymph nodes may be removed for biopsy.
PET scan (positron emission tomography scan): A procedure to find
malignant tumour cells in the body. A small amount of radionuclide glucose
(sugar) is injected into a vein. The PET scanner rotates around the body and
makes a picture of where glucose is being used in the body. Malignant tumour
cells show up brighter in the picture because they are more active and take up
more glucose than normal cells. The use of PET for staging oesophageal cancer is
being studied in clinical trials.
The following stages are used for oesophageal cancer:
Stage 0 (Carcinoma in Situ)
In stage 0, cancer is found only in the innermost layer of cells lining the
oesophagus. Stage 0 is also called carcinoma in situ.
Stage I
In stage I, cancer has spread beyond the innermost layer of cells to the next
layer of tissue in the wall of the oesophagus.
Stage II
Stage II oesophageal cancer is divided into stage IIA and stage IIB, depending
on where the cancer has spread.
Stage IIA: Cancer has spread to the layer of oesophageal muscle or to the
outer wall of the oesophagus.
Stage IIB: Cancer may have spread to any of the first three layers of the
oesophagus and to nearby lymph nodes.
Stage III
In stage III, cancer has spread to the outer wall of the oesophagus and may have
spread to tissues or lymph nodes near the oesophagus.
Stage IV
Stage IV oesophageal cancer is divided into stage IVA and stage IVB, depending
on where the cancer has spread.
Stage IVA: Cancer has spread to nearby or distant lymph nodes.
Stage IVB: Cancer has spread to distant lymph nodes and/or organs in other parts
of the body.
Recurrent Oesophageal Cancer
Recurrent oesophageal cancer is cancer that has recurred after it has been
treated. The cancer may come back in the oesophagus or in other parts of the
body.
There are different types of treatment for patients with oesophageal cancer.
Different types of treatment are available for patients with oesophageal cancer.
Some treatments are standard (the currently used treatment), and some are being
tested in clinical trials. Before starting treatment, patients may want to think
about taking part in a clinical trial. A treatment clinical trial is a research
study meant to help improve current treatments or obtain information on new
treatments for patients with cancer. When clinical trials show that a new
treatment is better than the ďstandardĒ treatment, the new treatment may become
the standard treatment.
Five types of standard treatment are used:
Surgery
Surgery is the most common treatment for cancer of the oesophagus. Part of the
oesophagus may be removed in an operation called an oesophagectomy. The doctor
will connect the remaining healthy part of the oesophagus to the stomach so the
patient can still swallow. A plastic tube or part of the intestine may be used
to make the connection. Lymph nodes near the oesophagus may also be removed and
viewed under a microscope to see if they contain cancer. If the oesophagus is
partly blocked by the tumour, an expandable metal stent (tube) may be placed
inside the oesophagus to help keep it open.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other
types of radiation to kill cancer cells. There are two types of radiation
therapy. External radiation therapy uses a machine outside the body to send
radiation toward the cancer. Internal radiation therapy uses a radioactive
substance sealed in needles, seeds, wires, or catheters that are placed directly
into or near the cancer. The way the radiation therapy is given depends on the
type and stage of the cancer being treated.
A plastic tube may be inserted into the oesophagus to keep it open during
radiation therapy. This is called intraluminal intubation and dilation.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer
cells, either by killing the cells or by stopping the cells from dividing. When
chemotherapy is taken by mouth or injected into a vein or muscle, the drugs
enter the bloodstream and can reach cancer cells throughout the body (systemic
chemotherapy). When chemotherapy is placed directly in the spinal column, a body
cavity such as the abdomen, or an organ, the drugs mainly affect cancer cells in
those areas. The way the chemotherapy is given depends on the type and stage of
the cancer being treated.
Laser therapy
Laser therapy is a cancer treatment that uses a laser beam (a narrow beam of
intense light) to kill cancer cells.
Electrocoagulation
Electrocoagulation is the use of an electric current to kill cancer cells.
Patients have special nutritional needs during treatment for oesophageal cancer.
Many people with oesophageal cancer find it hard to eat because they have
difficulty swallowing. The oesophagus may be narrowed by the tumour or as a side
effect of treatment. Some patients may receive nutrients directly into a vein.
Others may need a feeding tube (a flexible plastic tube that is passed through
the nose or mouth into the stomach) until they are able to eat on their own.
Treatment Options By Stage
Stage 0 Oesophageal Cancer (Carcinoma in Situ)
Treatment of stage 0 oesophageal cancer (carcinoma in situ) is usually surgery.
Stage I Oesophageal Cancer
Treatment of stage I oesophageal cancer may include the following:
Surgery.
Clinical trials of chemotherapy plus radiation therapy, with or without surgery.
Clinical trials of new therapies used before or after surgery.
Stage II Oesophageal Cancer
Treatment of stage II oesophageal cancer may include the following:
Surgery.
Clinical trials of chemotherapy plus radiation therapy, with or without surgery.
Clinical trials of new therapies used before or after surgery.
Stage III Oesophageal Cancer
Treatment of stage III oesophageal cancer may include the following:
Surgery.
Clinical trials of chemotherapy plus radiation therapy, with or without surgery.
Clinical trials of new therapies used before or after surgery.
Stage IV Oesophageal Cancer
Treatment of stage IV oesophageal cancer may include the following:
External or internal radiation therapy as palliative therapy to relieve symptoms
and improve quality of life.
Laser surgery or electrocoagulation as palliative therapy to relieve symptoms
and improve quality of life.
Chemotherapy.
Clinical trials of chemotherapy.
Treatment Options for Recurrent Oesophageal Cancer
Treatment of recurrent oesophageal cancer may include the following:
Use of any standard treatments as palliative therapy to relieve symptoms and
improve quality of life.
Clinical trials of new therapies used before or after surgery.
BACK
|
|
Gallbladder
Cancer Cancer of the gallbladder, an
uncommon cancer, is a disease in which cancer cells are found in the tissues of
the gallbladder. The gallbladder is a pear-shaped organ that lies just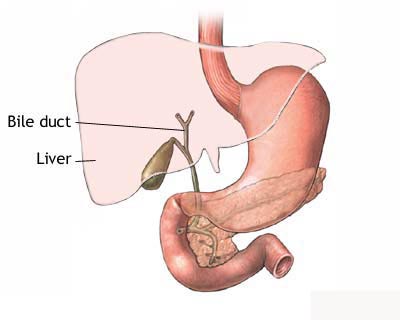 under the liver in the upper abdomen. Bile, a fluid made by the liver, is stored
in the gallbladder. When food is being broken down (digested) in the stomach and
the intestines, bile is released from the gallbladder through a tube called the
bile duct that connects the gallbladder and liver to the first part of the small
intestine. The bile helps to digest fat.
under the liver in the upper abdomen. Bile, a fluid made by the liver, is stored
in the gallbladder. When food is being broken down (digested) in the stomach and
the intestines, bile is released from the gallbladder through a tube called the
bile duct that connects the gallbladder and liver to the first part of the small
intestine. The bile helps to digest fat.
Cancer of the gallbladder is
more common in women than in men. It is also more common in people who have hard
clusters of material in their gallbladder (gallstones).
 Cancer of the gallbladder is
hard to find (diagnose) because the gallbladder is hidden behind other organs in
the abdomen. Cancer of the gallbladder is sometimes found after the gallbladder
is removed for other reasons. The symptoms of cancer of the gallbladder may be
like other diseases of the gallbladder, such as gallstones or infection, and
there may be no symptoms in the early stages. A doctor should be seen if the
following symptoms persist: Cancer of the gallbladder is
hard to find (diagnose) because the gallbladder is hidden behind other organs in
the abdomen. Cancer of the gallbladder is sometimes found after the gallbladder
is removed for other reasons. The symptoms of cancer of the gallbladder may be
like other diseases of the gallbladder, such as gallstones or infection, and
there may be no symptoms in the early stages. A doctor should be seen if the
following symptoms persist:
- Pain above the
stomach
- Loss of weight
without trying
- Fever
- Yellowing of the
skin (jaundice)
If there are symptoms, a doctor
may order x-rays and other tests to see what is wrong. However, usually the
cancer cannot be found unless the patient has surgery. During surgery, a cut is
made in the abdomen so that the gallbladder and other nearby organs and tissues
can be examined.
The chance of recovery and
choice of treatment depend on the stage of cancer (whether it is just in the
gallbladder or has spread to other places) and on the patientís general health.
Stage Explanation
Stages of cancer of the
gallbladder
Once cancer of the gallbladder
is found, more tests will be done to find out if cancer cells have spread to
other parts of the body. A doctor needs to know the stage to plan treatment. The
following stages are used for cancer of the gallbladder:
Localized
Cancer is found only in the
tissues that make up the wall of the gallbladder, and it can be removed
completely in an operation.
Unresectable
All of the cancer cannot be
removed in an operation. Cancer has spread to the tissues around the
gallbladder, such as the liver, stomach, pancreas, or intestine and/or to lymph
nodes in the area. (Lymph nodes are small, bean-shaped structures that are found
throughout the body. They produce and store infection-fighting cells.)
Recurrent
Recurrent disease means that
the cancer has come back (recurred) after it has been treated. It may come back
in the gallbladder or in another part of the body.
How cancer of the
gallbladder is treated
There are treatments for all
patients with cancer of the gallbladder. Three treatments are used:
- Surgery (taking
out the cancer or relieving symptoms of the cancer in an operation)
- Radiation
therapy (using high-dose x-rays to kill cancer cells)
- Chemotherapy
(using drugs to kill cancer)
Surgery is a common treatment
of cancer of the gallbladder if it has not spread to surrounding tissues. The
doctor may take out the gallbladder in an operation called a cholecystectomy.
Part of the liver around the gallbladder and lymph nodes in the abdomen may also
be removed.
If the cancer has spread and
cannot be removed, the doctor may do surgery to relieve symptoms. If the cancer
is blocking the bile ducts and bile builds up in the gallbladder, the doctor may
do surgery to go around (bypass) the cancer. During this operation, the doctor
will cut the gallbladder or bile duct and sew it to the small intestine. This is
called biliary bypass. Surgery or other procedures may also be done to put in a
tube (catheter) to drain bile that has built up in the area. During these
procedures, the doctor may place the catheter so that it drains through a tube
to the outside of the body or so that it goes around the blocked area and drains
the bile into the small intestine.
Radiation therapy is the use of
high-energy x-rays to kill cancer cells and shrink tumours. Radiation for
gallbladder cancer usually comes from a machine outside the body (external-beam
radiation therapy). Radiation may be used alone or in addition to surgery.
Chemotherapy is the use of
drugs to kill cancer cells. Chemotherapy for cancer of the gallbladder is
usually put into the body by a needle inserted into a vein. Chemotherapy is
called a systemic treatment because the drug enters the bloodstream, travels
through the body, and can kill cancer cells outside the gallbladder.
Chemotherapy or other drugs may be given with radiation therapy to make cancer
cells more sensitive to radiation (radiosensitizers).
Treatment by stage
Treatments for cancer of the
gallbladder depend on the stage of the disease and the patientís general health.
Localized
Gallbladder Cancer
Treatment may be one of the
following:
- Surgery to
remove the gallbladder and some of the tissues around it (cholecystectomy).
- External-beam
radiation therapy with or without chemotherapy, possibly followed by surgery.
- A clinical trial
evaluating radiation therapy plus chemotherapy or drugs to make the cancer
cells more sensitive to radiation (radiosensitizers).
Unresectable
Gallbladder Cancer
Treatment may be one of the
following:
- Surgery or other
procedures to relieve symptoms.
- Surgery to
bypass the obstructed ducts of the gallbladder.
- External-beam
radiation therapy with or without chemotherapy possibly followed by surgery.
- Chemotherapy to
relieve symptoms. Clinical trials are testing new chemotherapy drugs.
- A clinical trial
evaluating radiation therapy plus chemotherapy or drugs to make the cancer
cells more sensitive to radiation (radiosensitizers).
Recurrent
Gallbladder Cancer
Treatment for recurrent cancer
of the gallbladder depends on the type of treatment the patient received before,
the place where the cancer has recurred and other facts about the cancer, and
the patientís general health. The patient may wish to consider taking part in a
clinical trial.
BACK
|
|
Liver Cancer
The liver is the largest of the body's organs.
It lies in the upper right side of the abdomen, with most of it protected by the
ribs It weighs about 3 pounds (1.5 kilogrammes), making it the largest organ in
the body. It pulses continuously as 1 1/2 litres (2 1/2 pints) of blood pass
through it every minute. There are reservoirs of blood in the liver called
venous sinuses which can hold up to 3 1/2 litres (6 pints) for boosting blood
volume in emergencies.
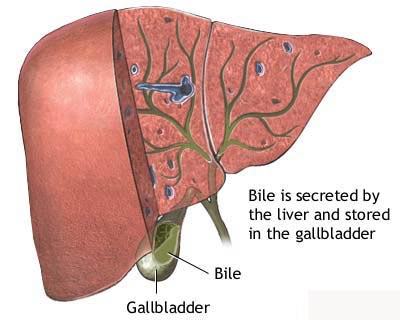 The
liver is a 24 hour chemical plant responsible for the production, storage,
metabolism and distribution of a multitude of nutrients essential to a healthy
body. It takes in waste products, converts some of them into useable elements
and excretes those which are harmful. At the same time the liver produces
Vitamin A and stores Vitamins A, D and B12. A chemical company would require a
plant covering several acres to perform its simpler tasks. The more complicated
ones it could not do at all. The
liver is a 24 hour chemical plant responsible for the production, storage,
metabolism and distribution of a multitude of nutrients essential to a healthy
body. It takes in waste products, converts some of them into useable elements
and excretes those which are harmful. At the same time the liver produces
Vitamin A and stores Vitamins A, D and B12. A chemical company would require a
plant covering several acres to perform its simpler tasks. The more complicated
ones it could not do at all.
Adult primary liver cancer is a
disease in which malignant cells form in the tissues of the liver. The liver is
one of the largest organs in the body, filling the upper right side of the
abdomen inside the rib cage. It has two parts, a right lobe and a smaller left
lobe. The liver makes enzymes and bile that help digest food and change it into
energy. The liver also filters and stores blood.
This summary refers to the treatment of primary liver cancer (cancer that begins
in the liver). Treatment of metastatic liver cancer, which is cancer that begins
in other parts of the body and spreads to the liver, is not discussed in this
summary. Primary liver cancer can occur in both adults and children. Treatment
for children, however, is different than treatment for adults.
Having hepatitis or cirrhosis can affect the risk of developing adult primary
liver cancer.
The following are possible risk factors for adult primary liver cancer:
- Having hepatitis B
and/or hepatitis C
- Having a close relative
with both hepatitis and liver cancer
- Having cirrhosis
- Eating foods tainted with aflatoxin
(poison from a fungus that can grow on foods, such as grains and
nuts, that have not been stored properly)
- Possible signs of adult
primary liver cancer include a lump or pain on the right side
These symptoms may be caused by swelling of the liver. These and other symptoms
may be caused by adult primary liver cancer or by other conditions. A doctor
should be consulted if any of the following problems occur:
-
A hard lump
on the right side just below the rib cage
-
Discomfort
in the upper abdomen on the right side
-
Pain around
the right shoulder blade
-
Unexplained
weight loss
-
Jaundice
(yellowing of the skin and whites of the eyes)
-
Unusual
tiredness
-
Nausea
-
Loss of appetite.
Tests that examine the liver
and the blood are used to detect (find) and diagnose adult primary liver cancer. The following tests and procedures may be used:
- Physical exam and history: An exam of the body to check general signs of health,
including checking for signs of disease, such as lumps or anything else that
seems unusual. A history of the patientís health habits and past illnesses and
treatments will also be taken.
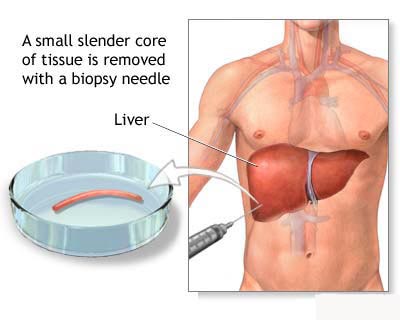
- Blood chemistry studies: A procedure in which a blood sample is checked to
measure the amounts of certain substances released into the blood by organs and
tissues in the body. An unusual (higher or lower than normal) amount of a
substance can be a sign of disease in the organ or tissue that produces it. An
increased level of alpha-fetoprotein (AFP) in the blood may be a sign of liver
cancer. Other cancers and certain non-cancerous conditions, including cirrhosis
and hepatitis, may also increase AFP levels.
Complete blood count: A procedure in which a sample of blood is drawn and
checked for the following:
- The number of red blood
cells, white blood cells, and platelets
- The amount of haemoglobin (the protein that carries oxygen) in the red blood
cells. The portion of the sample made up of red blood cells
- Laparoscopy: A surgical procedure to look at the organs inside the abdomen to
check for abnormal areas. An incision (cut) is made in the abdominal wall and a
laparoscope (a thin, lighted tube) is inserted into the abdomen. Tissue samples
and lymph nodes may be removed for biopsy.
Biopsy: The removal of cells or tissues so they can be viewed under a microscope
to check for signs of cancer. The sample may be taken using a fine needle
inserted into the liver during an x-ray or ultrasound. This is called needle
biopsy or fine-needle aspiration. The biopsy may be done during a laparoscopy.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of
areas inside the body, taken from different angles. The pictures are made by a
computer linked to an x-ray machine. A dye may be injected into a vein or
swallowed to help the organs or tissues show up more clearly. This procedure is
also called computed tomography, computerized tomography, or computerized axial
tomography.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves,
and a computer to make a series of detailed pictures of areas inside the body.
This procedure is also called nuclear magnetic resonance imaging (NMRI).
- Ultrasound: A procedure in which high-energy sound waves (ultrasound) are
bounced off internal tissues or organs and make echoes. The echoes form a
picture of body tissues called a sonogram.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) and treatment options depend on the
following:
- The stage of the cancer (the
size of the tumour, whether it affects part or all of the liver, or has spread
to other places in the body).
- How well the liver is
working.
- The patientís general
health, including whether there is cirrhosis of the liver.
Prognosis is also affected by
alpha-fetoprotein (AFP) levels.
After adult primary liver cancer has been diagnosed, tests are done to find out
if cancer cells have spread within the liver or to other parts of the body.
The process used to find out if cancer has spread within the liver or to other
parts of the body is called staging. The information gathered from the staging
process determines the stage of the disease. It is important to know the stage
in order to plan treatment. The following tests and procedures may be used in
the staging process:
Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray
is a type of energy beam that can go through the body and onto film, making a
picture of areas inside the body.
CT scan (CAT scan): A
procedure that makes a series of detailed pictures of areas inside the body,
taken from different angles. The pictures are made by a computer linked to an
x-ray machine. A dye may be injected into a vein or swallowed to help the organs
or tissues show up more clearly. This procedure is also called computed
tomography, computerized tomography, or computerized axial tomography.
MRI (magnetic resonance imaging): A procedure that uses a magnet, radio
waves, and a computer to make a series of detailed pictures of areas inside the
body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
Bone scan: A procedure
to check if there are rapidly dividing cells, such as cancer cells, in the bone.
A very small amount of radioactive material is injected into a vein and travels
through the bloodstream. The radioactive material collects in the bones and is
detected by a scanner.
Doppler ultrasound: A
type of ultrasound that uses differences in the ultrasound echoes to measure the
speed and direction of blood flow.
The following stages are used
for adult primary liver cancer:
Stage I
In stage I, there is one tumour and it has not spread to nearby blood vessels.
Stage II
In stage II, one of the following is found: one tumour that has spread to nearby
blood vessels; or more than one tumour, none of which is larger than 5
centimetres (about 2 inches).
Stage III
Stage III is divided into stage IIIA, IIIB, and IIIC.
Stage IIIA: In stage IIIA, one of the following is found: more than one tumour
larger than 5 centimetres; or one tumour that has spread to a major branch of
blood vessels near the liver.
Stage IIIB: In stage IIIB, there are one or more tumours of any size that have
either: spread to nearby organs other than the gallbladder; or broken through
the lining of the peritoneal cavity.
Stage IIIC: In stage IIIC, the cancer has spread to nearby lymph nodes.
Stage IV
In stage IV, cancer has spread beyond the liver to other places in the body,
such as the bones or lungs. The tumours may be of any size and may also have
spread to nearby blood vessels and/or lymph nodes.
For adult primary liver cancer, stages are also grouped according to how the
cancer may be treated. There are 3 treatment groups:
Localized resectable
The cancer is found in the liver only, has not spread, and can be completely
removed by surgery.
Localized and locally advanced unresectable
The cancer is found in the liver only and has not spread, but cannot be
completely removed by surgery.
Advanced
Cancer has spread throughout the liver or has spread to other parts of the body,
such as the lungs and bone.
There are different types of
treatment for patients with adult primary liver cancer.
Different types of
treatments are available for patients with adult
primary
liver cancer. Some treatments are standard (the
currently used treatment), and some are being tested in
clinical trials. Before starting treatment, patients
may want to think about taking part in a clinical trial. A treatment clinical
trial is a research study meant to help improve current treatments or obtain
information on new treatments for patients with
cancer. When clinical trials show that a new treatment
is better than the
ďstandardĒ treatment, the new treatment may become the
standard treatment.
Four types of standard
treatment are used:
Surgery
The following types of
surgery may be used to treat liver cancer:
-
Cryosurgery: A
treatment that uses an instrument to freeze and destroy
abnormal
tissue, such as
carcinoma in situ (cancer that involves only the
cells in which it began and that has not spread to
nearby tissues). This type of treatment is also called cryotherapy. The doctor
may use ultrasound to guide the instrument.
- Partial
hepatectomy: Removal of the part of the liver where
cancer is found. The part removed may be a wedge of tissue, an entire
lobe, or a larger portion of the liver, along with
some of the healthy tissue around it. The remaining liver tissue takes over
the functions of the liver.
- Total
hepatectomy and liver
transplant: Removal of the entire liver and
replacement with a healthy donated liver. A liver transplant may be done when
the disease is in the liver only and a donated liver can be found. If the
patient has to wait for a donated liver, other treatment is given as needed.
-
Radiofrequency ablation:
The use of a special probe with tiny electrodes that kill cancer cells.
Sometimes the probe is inserted directly through the skin and only
local anaesthesia is needed. In other cases, the
probe is inserted through an
incision in the
abdomen. This is done in the hospital with
general anaesthesia.
Radiation therapy
Radiation therapy
is a cancer treatment that uses high-energy
x-rays or other types of
radiation to kill cancer cells. Radiation therapy is
given in different ways:
-
External radiation
therapy uses a machine outside the body to send radiation toward the cancer.
-
Internal radiation
therapy uses a
radioactive substance sealed in needles,
seeds, wires, or
catheters that are placed directly into or near the
cancer.
- Drugs
called
radio sensitizers may be given with the radiation
therapy to make the cancer cells more sensitive to radiation.
- Radiation
may be delivered to the
tumour using
radio-labelled
antibodies. Radioactive substances are attached to
antibodies made in the laboratory. These antibodies, which target tumour
cells, are
injected into the body and the tumour cells are
killed by the radioactive substance.
The way the radiation
therapy is given depends on the type and
stage of the cancer being treated.
Chemotherapy
Chemotherapy is a
cancer treatment that uses drugs to stop the growth of cancer cells, either by
killing the cells or by stopping the cells from dividing. When chemotherapy is
taken by mouth or injected into a vein or muscle, the drugs enter the
bloodstream and can reach cancer cells throughout the body (systemic
chemotherapy). When chemotherapy is placed directly
into the spinal column, a body cavity such as the abdomen, or an
organ, the drugs mainly affect cancer cells in those
areas. This is called
regional chemotherapy.
Regional chemotherapy is
usually used to treat liver cancer. A small pump containing anticancer drugs may
be placed in the body. The pump puts the drugs directly into the
blood vessels that go to the tumour.
Another type of regional
chemotherapy is
chemo-embolization of the
hepatic artery. This involves blocking the hepatic
artery (the main artery that supplies
blood to the liver) and injecting anticancer drugs
between the blockage and the liver. The liverís arteries then deliver the drugs
throughout the liver. Only a small amount of the drug reaches other parts of the
body. The blockage may be temporary or permanent, depending on what is used to
block the artery. The liver continues to receive some blood from the
hepatic portal vein, which carries blood from the
stomach and
intestine.
The way the chemotherapy is
given depends on the type and stage of the cancer being treated.
Percutaneous ethanol injection
Percutaneous ethanol injection
is a cancer treatment in which a small needle is used to inject ethanol
(alcohol) directly into a tumour to kill cancer cells. The procedure may be done
once or twice a week. Usually local anaesthesia is used, but if the patient has
many tumours in the liver, general anaesthesia may be needed.
Other types of treatment are
being tested in clinical trials. These include the following:
Hyperthermia therapy
Hyperthermia therapy is
the use of a special machine to heat the body for a period of time to kill
cancer cells. Because some cancer cells are more sensitive to heat than normal
cells are, the cancer cells die and the tumour shrinks.
Biologic therapy
Biologic therapy
is treatment that uses the patientís
immune system to fight cancer. Substances made by the
body or made in a laboratory are used to boost, direct, or restore the bodyís
natural defences against disease. This type of cancer treatment is also called
biotherapy or immunotherapy.
Treatment Options for Adult
Primary Liver Cancer
Localized Resectable Adult Primary Liver Cancer
Treatment of localized resectable adult primary liver cancer may include the
following:
Surgery (partial hepatectomy).
Surgery (total hepatectomy) and liver transplant.
Localized and Locally Advanced Unresectable Adult Primary Liver Cancer
Treatment of localized and locally advanced unresectable adult primary liver
cancer may include the following:
Chemotherapy (regional chemotherapy or chemo-embolization).
Surgery (cryosurgery or radiofrequency ablation).
Surgery (total hepatectomy) and liver transplant.
Percutaneous ethanol injection.
Radiation therapy with radio sensitizers.
A clinical trial of regional or systemic chemotherapy and/or radio-labelled
antibodies.
A clinical trial of a combination of surgery, chemotherapy, and radiation
therapy. Hyperthermia therapy may also be used. Chemotherapy and radiation
therapy may be used to shrink the tumour before surgery.
Advanced Adult Primary Liver Cancer
There is no standard treatment for advanced adult primary liver cancer. Patients
may consider taking part in a clinical trial. Treatment may include the
following:
A clinical trial of biologic therapy, chemotherapy, and/or radiation therapy
with or without radio sensitizers. These treatments may be given as palliative
therapy to help relieve symptoms and improve the quality of life.
Recurrent Adult Primary Liver Cancer
Treatment of recurrent adult primary liver cancer may include the following:
Surgery (partial hepatectomy).
Surgery (total hepatectomy) and liver transplant.
Chemotherapy (chemo-embolization or systemic chemotherapy).
Percutaneous ethanol injection.
A clinical trial of a new therapy.
BACK
|
Pancreatic
Cancer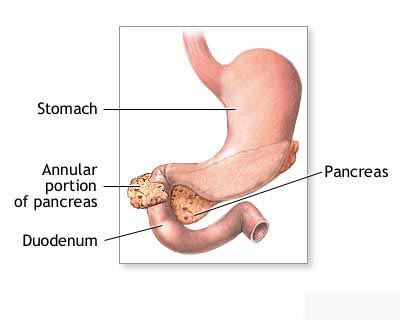
Pancreatic cancer is a disease
in which malignant cells form in the tissues of the pancreas. The pancreas is a
gland about 6 inches long that is shaped like a thin pear lying on its side. The
wider end of the pancreas is called the head, the middle section is called the
body, and the narrow end is called the tail. The pancreas lies behind the
stomach and in front of the spine.
The pancreas has two main jobs in the body:
- To produce juices that help digest (break down) food.
- To produce hormones, such as insulin and glucagon, that help control blood sugar
levels. Both of these hormones help the body use and store the energy it gets
from food.
- The digestive juices are produced by exocrine pancreas cells and the hormones
are produced by endocrine pancreas cells. About 95% of pancreatic cancers begin
in exocrine cells.
- Smoking and health history can affect the risk of developing pancreatic cancer.
The following are possible risk factors for pancreatic cancer:
- Smoking
- Long-standing diabetes
- Chronic pancreatitis
- Certain hereditary conditions, such as
hereditary pancreatitis, multiple endocrine neoplasia type 1 syndrome,
hereditary nonpolyposis colon cancer (HNPCC; Lynch syndrome), von
Hippel-Lindau syndrome, ataxia-telangiectasia, and the familial atypical
multiple mole melanoma syndrome (FAMMM)
Possible
signs of pancreatic cancer include jaundice, pain, and weight loss.
These symptoms can be caused by pancreatic cancer or other conditions. A doctor
should be consulted if any of the following problems occur:
- Jaundice (yellowing of
the skin and whites of the eyes)
- Pain in the upper or
middle abdomen and back
- Unexplained weight loss
- Loss of appetite
- Fatigue
Pancreatic cancer is difficult to detect
(find) and diagnose early. Pancreatic cancer is difficult to detect and diagnose
for the following reasons:
- There arenít any noticeable signs or
symptoms in the early stages of pancreatic cancer
- The signs of pancreatic cancer, when
present, are like the signs of many other illnesses
- The pancreas is hidden behind other organs
such as the stomach, small intestine, liver, gallbladder, spleen, and bile
ducts
Tests that examine the pancreas are used to
detect, diagnose and stage pancreatic cancer.
Pancreatic cancer is usually diagnosed with tests and procedures that produce
pictures of the pancreas and the area around it. The process used to find out if
cancer cells have spread within and around the pancreas is called staging. Tests
and procedures to detect, diagnose, and stage pancreatic cancer are usually done
at the same time. In order to plan the best treatment, it is important to know
the stage of the disease and whether or not the pancreatic cancer can be removed
by surgery. The following tests and procedures may be used:
Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray
is a type of energy beam that can go through the body and onto film, making a
picture of areas inside the body.
Physical exam and history: An exam of the body to check general signs of
health, including checking for signs of disease, such as lumps or anything else
that seems unusual. A history of the patientís health habits and past illnesses
and treatments will also be taken.
CT scan (CAT scan): A procedure that makes a series of detailed pictures
of areas inside the body, taken from different angles. The pictures are made by
a computer linked to an x-ray machine. A dye may be injected into a vein or
swallowed to help the organs or tissues show up more clearly. This procedure is
also called computed tomography, computerized tomography, or computerized axial
tomography. A spiral or helical CT scan takes detailed pictures of areas inside
the body as it scans the body in a spiral path.
MRI (magnetic resonance imaging): A procedure that uses a magnet, radio
waves, and a computer to make a series of detailed pictures of areas inside the
body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
PET scan (positron emission tomography scan): A procedure to find
malignant tumour cells in the body. A small amount of radionuclide glucose
(sugar) is injected into a vein. The PET scanner rotates around the body and
makes a picture of where glucose is being used in the body. Malignant tumour
cells show up brighter in the picture because they are more active and take up
more glucose than normal cells.
Endoscopic ultrasound (EUS): A procedure in which an endoscope (a thin,
lighted tube) is inserted into the body. The endoscope is used to bounce
high-energy sound waves (ultrasound) off internal tissues or organs and make
echoes. The echoes form a picture of body tissues called a sonogram. This
procedure is also called endosonography.
Laparoscopy: A surgical procedure to look at the organs inside the abdomen
to check for abnormal areas. An incision (cut) is made in the abdominal wall and
a laparoscope (a thin, lighted tube) is inserted into the abdomen. Tissue
samples and lymph nodes may be removed for biopsy.
Endoscopic retrograde cholangiopancreatography (ERCP): A procedure used
to x-ray the ducts (tubes) that carry bile from the liver to the gallbladder and
from the gallbladder to the small intestine. Sometimes pancreatic cancer causes
these ducts to narrow and block or slow the flow of bile, causing jaundice. An
endoscope (a thin, lighted tube) is passed through the mouth, oesophagus, and
stomach into the first part of the small intestine. A catheter (a smaller tube)
is then inserted through the endoscope into the pancreatic ducts. A dye is
injected through the catheter into the ducts and an x-ray is taken. If the ducts
are blocked by a tumour, a fine tube may be inserted into the duct to unblock
it. This tube (or stent) may be left in place to keep the duct open. Tissue
samples may also be taken.
Percutaneous transhepatic cholangiography (PTC): A procedure used to
x-ray the liver and bile ducts. A thin needle is inserted through the skin below
the ribs and into the liver. Dye is injected into the liver or bile ducts and an
x-ray is taken. If a blockage is found, a thin, flexible tube called a stent is
sometimes left in the liver to drain bile into the small intestine or a
collection bag outside the body. This test is done only if ERCP cannot be done.
Biopsy: The removal of cells or tissues so they can be viewed under a
microscope to check for signs of cancer. There are several ways to do a biopsy
for pancreatic cancer. A fine needle may be inserted into the pancreas during an
x-ray or ultrasound to remove cells. Tissue may also be removed during a
laparoscopy (a surgical incision made in the wall of the abdomen).
Certain factors affect treatment options and prognosis (chance of recovery).
The treatment options and prognosis (chance of recovery) depend on the stage of
the cancer (the size of the tumour and whether the cancer has spread outside the
pancreas to nearby tissues or lymph nodes or to other places in the body) and
the patientís general health. Lymph nodes are small, bean-shaped structures
found throughout the body. They filter substances in a fluid called lymph and
help fight infection and disease.
Pancreatic cancer can be controlled only if it is found before it has spread,
when it can be removed by surgery. If the cancer has spread, palliative
treatment can improve the quality of life by controlling the symptoms and
complications of this disease.
Tests and
procedures to stage pancreatic cancer are usually done at the same time as
diagnosis.
The following stages are used for
pancreatic cancer:
Stage I
In stage I,
cancer is found in the
pancreas only. Stage I is divided into stage IA and
stage IB, depending on where the cancer has spread.
- Stage IA: Cancer is found only
in the pancreas and is 2 centimetres or less in size.
- Stage IB: Cancer is found only
in the pancreas and is greater than 2 centimetres in size.
Stage II
In
stage II, cancer may have spread to nearby
tissue and
organs, and may have spread to
lymph nodes near the pancreas. Stage II is divided
into stage IIA and stage IIB, depending on where the cancer has spread.
- Stage IIA: Cancer has spread to
nearby tissue and organs but has not spread to nearby lymph nodes.
- Stage IIB: Cancer has spread to
nearby lymph nodes and may have spread to nearby tissue and organs.
Stage III
In
stage III, cancer has spread to the major blood
vessels near the pancreas, such as the celiac axis (the junction where the
celiac artery branches off from the
aorta, just below the diaphragm) and the superior
mesenteric vein (the vein that returns blood from the
rectum and
colon to the heart) and aorta, and may have spread to
nearby lymph nodes.
Stage IV
In
stage IV, cancer may be of any size and has spread to
distant organs, such as the liver, lung, and
peritoneal cavity (the body cavity that contains most
of the organs in the
abdomen (such as the lungs). It may have also spread
to organs and tissues near the pancreas or to lymph nodes.
There are different types of treatment for
patients with pancreatic cancer.
Different types of treatment are
available for patients with pancreatic
cancer. Some treatments are standard (the currently
used treatment), and some are being tested in
clinical trials. Before starting treatment, patients
may want to think about taking part in a clinical trial. A treatment clinical
trial is a research study meant to help improve current treatments or obtain
information on new treatments for patients with cancer. When clinical trials
show that a new treatment is better than the
ďstandardĒ treatment, the new treatment may become the
standard treatment.
Three types of standard treatment are used:
Surgery
One of the following types of
surgery may be used to take out the
tumour:
-
Whipple procedure:
A surgical procedure in which the head of the
pancreas, the
gallbladder, part of the
stomach, part of the
small intestine, and the bile duct are removed.
Enough of the pancreas is left to produce digestive juices and
insulin.
-
Total pancreatectomy:
This operation removes the whole pancreas, part of the stomach, part of the
small intestine, the
common bile duct, the gallbladder, the
spleen, and nearby
lymph nodes.
- Distal pancreatectomy: The body
and the tail of the pancreas and usually the spleen are removed.
If the cancer has spread and cannot be
removed, the following types of
palliative surgery may be done to relieve symptoms:
- Surgical
biliary
bypass: If cancer is blocking the small intestine
and
bile is building up in the gallbladder, a biliary
bypass may be done. During this operation, the doctor will cut the gallbladder
or bile duct and sew it to the small intestine to create a new pathway around
the blocked area.
-
Endoscopic
stent placement: If the tumour is blocking the bile
duct, surgery may be done to put in a stent (a thin tube) to drain bile that
has built up in the area. The doctor may place the stent through a
catheter that drains to the outside of the body or
the stent may go around the blocked area and drain the bile into the small
intestine.
-
Gastric bypass: If
the tumour is blocking the flow of food from the stomach, the stomach may be
sewn directly to the small intestine so the patient can continue to eat
normally.
Radiation therapy
Radiation therapy
is a cancer treatment that uses high-energy
x-rays or other types of
radiation to kill cancer
cells. There are two types of radiation therapy.
External radiation therapy uses a machine outside the
body to send radiation toward the cancer.
Internal radiation therapy uses a
radioactive substance sealed in needles,
seeds, wires, or catheters that are placed directly
into or near the cancer. The way the radiation therapy is given depends on the
type and stage of the cancer being treated.
Chemotherapy
Chemotherapy is a
cancer treatment that uses drugs to stop the growth of cancer cells, either by
killing the cells or by stopping the cells from dividing. When chemotherapy is
taken by mouth or
injected into a vein or muscle, the drugs enter the
bloodstream and can reach cancer cells throughout the body (systemic
chemotherapy). When chemotherapy is placed directly in
the spinal column, a body cavity such as the
abdomen, or an
organ, the drugs mainly affect cancer cells in those
areas. The way the chemotherapy is given depends on the type and stage of the
cancer being treated.
Other types of treatment are being tested in
clinical trials.
Biologic therapy
Biologic therapy
is a treatment that uses the patientís immune system to fight cancer. Substances
made by the body or made in a laboratory are used to boost, direct, or restore
the bodyís natural defences against cancer. This type of cancer treatment is
also called
biotherapy or
immunotherapy.
There are treatments for pain caused by
pancreatic cancer.
Pain can occur when the tumour presses
on nerves or other organs near the pancreas. When pain medicine is not enough,
there are treatments that act on nerves in the
abdomen to relieve the pain. The doctor may inject
medicine into the area around affected nerves or may cut the nerves to block the
feeling of pain. Radiation therapy with or without chemotherapy can also help
relieve pain by shrinking the tumour.
Patients with
pancreatic cancer have special nutritional needs.
Surgery to remove the pancreas may
interfere with the production of
pancreatic enzymes that help to digest food. As a
result, patients may have problems digesting food and absorbing nutrients into
the body. To prevent
malnutrition, the doctor may prescribe medicines that
replace these enzymes.
Treatment Options By Stage
Stage I Pancreatic Cancer
Treatment of stage I pancreatic cancer may include the following:
Surgery alone.
Surgery with chemotherapy and radiation therapy.
A clinical trial of surgery followed by radiation therapy with chemotherapy.
Chemotherapy is given before, during, and after the radiation therapy.
Stage IIA Pancreatic Cancer
Treatment of stage IIA pancreatic cancer may include the following:
Surgery with or without chemotherapy and radiation therapy.
Radiation therapy with chemotherapy.
Palliative surgery to bypass blocked areas in ducts or the small intestine.
A clinical trial of surgery followed by radiation therapy with chemotherapy.
Chemotherapy is given before, during, and after the radiation therapy.
A clinical trial of radiation therapy combined with chemotherapy and/or
radiosensitizers (drugs that make cancer cells more sensitive to radiation so
more tumor cells are killed), followed by surgery.
A clinical trial of chemotherapy.
A clinical trial of radiation therapy given during surgery or internal radiation
therapy.
Stage IIB Pancreatic Cancer
Treatment of stage IIB pancreatic cancer may include the following:
Surgery with or without chemotherapy and radiation therapy.
Radiation therapy with chemotherapy.
Palliative surgery to bypass blocked areas in ducts or the small intestine.
A clinical trial of surgery followed by radiation therapy with chemotherapy.
Chemotherapy is given before, during, and after the radiation therapy.
A clinical trial of radiation therapy combined with chemotherapy and/or
radiosensitizers (drugs that make cancer cells more sensitive to radiation so
more tumor cells are killed), followed by surgery.
A clinical trial of chemotherapy.
A clinical trial of radiation therapy given during surgery or internal radiation
therapy.
Stage III Pancreatic Cancer
Treatment of stage III pancreatic cancer may include the following:
Surgery with or without chemotherapy and radiation therapy.
Radiation therapy with chemotherapy.
Palliative surgery or stent placement to bypass blocked areas in ducts or the
small intestine.
A clinical trial of surgery followed by radiation therapy with chemotherapy.
Chemotherapy is given before, during, and after the radiation therapy.
A clinical trial of radiation therapy combined with chemotherapy and/or
radiosensitizers, followed by surgery.
A clinical trial of chemotherapy.
A clinical trial of radiation therapy given during surgery or internal radiation
therapy.
Stage IV Pancreatic Cancer
Treatment of stage IV pancreatic cancer may include the following:
Chemotherapy.
Palliative treatments for pain, such as nerve blocks, and other supportive care.
Palliative surgery or stent placement to bypass blocked areas in ducts or the
small intestine.
Clinical trials of chemotherapy or biological therapy.
Treatment Options for Recurrent Pancreatic Cancer
Treatment of recurrent pancreatic cancer may include the following:
Chemotherapy.
Palliative surgery to bypass blocked areas in ducts or the small intestine.
Palliative radiation therapy.
Other palliative medical care to reduce symptoms, such as nerve blocks to
relieve pain.
Clinical trials of chemotherapy or biological therapy.
BACK
|
| What is a
colostomy?
A colostomy, or stoma, is an artificial
opening created when a healthy part of your large bowel is brought out onto the
surface of your abdomen.
What does the large bowel do?
Your bowel is a hollow tube coiled up in your
abdomen. It is a part of the gut, which breaks down the food you eat into
protein for growth, and energy.
 When the food has been digested, waste
products pass into the large bowel. In the colon, the first part, water
is absorbed back into the body. The waste products become more solid and are
passed out of the body through the rectum (back passage) as faeces or
stools. When the food has been digested, waste
products pass into the large bowel. In the colon, the first part, water
is absorbed back into the body. The waste products become more solid and are
passed out of the body through the rectum (back passage) as faeces or
stools.
What happens when a colostomy is formed?
When a colostomy is formed your stools will be
passed through the stoma instead of through your rectum. The stoma has no muscle
control and you will wear an appliance (bag) to collect the stools.
What does a colostomy look like?
The colostomy may be oval or round in shape.
It is similar in colour to the lining to the lining of your mouth. The stoma
will be about two finger breadths across - three to four centimetres. It may be
swollen at first but this will settle in about seven to 10 days.
Although the stoma may stand out a couple of
centimetres from the surface of your abdomen, other people won't notice this
when you are dressed.
Are there different types of colostomy?
Yes, a colostomy may be temporary or
permanent.
A temporary colostomy may be formed to:
- relieve a blockage in the bowel. Other
treatment may be given to remove the blockage and start the bowel working
normally again.
- rest your bowel and allow healing to take
place after an operation.
A permanent colostomy will be formed if a
cancer is sited low in your rectum and there isn't enough bowel left to join
together after the tumour has been removed.
Examinations of your bowel
There are several ways in which the doctor can examine your
bowel. Whatever examination is used your bowel will need to be prepared. It must
be as empty as possible so that the doctor can get a clear view inside.
The preparation may vary but will usually include:
- eating a low fibre (roughage) diet for a day or so before
the test to clear your bowel of any residue. You may also be asked to drink
clear fluids only the day before the examination.
- taking laxatives to clear your upper bowel.
- an enema to make sure the lower part of the bowel is empty
Sigmoidoscopy or Colonscopy:
During these investigations the doctor passes a scope, a tube with a small
camera on the end, into your bowel. A sigmoidoscopy looks at the lower part of
your large bowel, while a colonscopy looks further up the colon.
The doctor can see if there is part of the lining of the bowel
which looks different, for example there may be a polyp (a small smooth growth)
or an ulcer.
If the doctor sees something unusual, a biopsy (a
sample of tissue) will be taken from this area. The tissue will be sent to the
laboratory for examination under the microscope.
Before these examinations you will be given something to make
you more relaxed and prevent any discomfort. If you have any questions, please
ask your doctor or nurse.
Barium Enema: This is an x-ray
examination using barium which brightens the x-ray picture. The barium is given
as an enema and will outline the lower part of your bowel. The procedure lasts
about 15-30 minutes and you should try to hold on to the contents of the enema
for the length of the examination.
Afterwards you will be able to empty your bowels. You may be
prescribed a mild laxative because barium can cause constipation. Barium can
also be very difficult to flush away in the toilet. If you have any questions,
please ask your doctor or nurse.
What happens before the operation?
You will usually be admitted to hospital two
or three days before your operation. This gives you time to get used to the ward
and to meet the staff who will be looking after you.
You will usually be given a light diet for 24
hours, followed by fluids only for the next 24 hours in the two days before your
operation. You will then be asked not to eat or drink for several hours.
You will be given a laxative and / or enema to
make sure your bowel is empty
A stoma care nurse will visit you. S/he is a
specialist nurse trained to help people with colostomies. The nurse will mark
the site of your colostomy on your abdomen with a pen. The site will be
discussed with you to make sure it is an easy place for you to manage, for
example to change your appliance. The nurse will also make sure that the site is
away from your naval, hip bones and creases.
The stoma care nurse will show you some of the
available appliances and may leave you a general information booklet. S/he can
also discuss all aspects of your operation and any concerns you may have about
how having a colostomy will affect your life.
What happens after the operation?
After your operation you will be taken to the
recovery room. Here the nurses can check you closely while you are waking up.
When the anaesthetist is satisfied with your condition, you will be taken back
to your ward.
People experience pain in different ways and
at different levels. If you do feel sore or uncomfortable, please tell the
nurses straight away. They can give you some analgesia (pain relief) and, if you
are felling sick, some anti-emetic (anti-sickness) drugs. During your operation the surgeon has to
handle your bowel and, because of this, it takes some time to start working
normally again. You won't be able to drink or eat at first but gradually you
will begin to take fluids and food again. You will probably be eating normally
seven to ten days after your operation.
You will also have a thin tube inserted up
your noise and down into your stomach. This is to drain off any fluid and stop
you from being sick. It won't affect your ability to speak. You will be given fluids, and any drugs you
need, by an infusion ('drip') into a vein, usually in your arm. This will stay
in place for a few days until you are able to drink normally again. A catheter (tube) will be placed in your
bladder to drain away urine and prevent you from becoming uncomfortable. This
won't be left in place any longer than necessary.
When any tissue is cut it is normal for blood
and fluid to be produced. You may have a wound drain (tube) in place to remove
this. Your wound will be stitched together and your nurse will tell you when the
stitches can be removed. If you have had your rectum removed, your back
passage may be stitched together or a wound drain may be in place. The drain
will be removed after a few days. A little discharge or bleeding may continue
for several weeks while the area is healing. You will be encouraged to get up and move
around, with help, within 24 hours of your operation.
Care of your colostomy
Your colostomy may be swollen for the first
week or 10 days because your bowel was handled during the operation. For the
same reason your colostomy may not function for a few days. However, you may
pass wind in the bag which means your bowel is recovering.
At first the nurses will look after your
colostomy and then they will teach you to do this. Gradually you will learn how
to change your bag, dispose of used ones and care for your skin. You will be
able to select an appliance which suits you.
You will be able to go home when you feel
confident changing your bag and looking after your colostomy, and after your
stitches have been removed. Your colostomy will continue to shrink in size
during the six weeks after your operation.
How am I likely to feel?
Many people find it takes time, and support
from others, to adjust to living with a stoma. As well as this, you may be
experiencing many different emotions following your diagnosis of cancer.
Your feelings may change from day to day and
it isn't unusual to have 'up' days and 'down' days. It may take several weeks or
months to feel you have really adjusted physically and emotionally to what has
happened. After any operation people often feel tired and sometimes depressed or
low. This is normal.
Some people say they lost their self
confidence at this time, either related to life in general or feelings about the
change to their body caused by the formation of the stoma. If you feel like
this, talk to your partner or others close to you. A lot of people say this has
helped them to regain their confidence and to realise they are the same person
as before their operation and valued as such. All these reactions are
normal.
Will I look different?
You may be concerned that you'll look
different after the formation of your stoma. Don't worry, it's unlikely that
people will know about your operation unless you tell them. There is no reason why you should need to
change your wardrobe or buy different clothes. Occasionally some change may be
necessary if you have a transverse colostomy because of the position of the
stoma. Specialist swim wear is available but, again,
may not be necessary.
What about my usual activities?
Having a colostomy shouldn't prevent you from
doing many of the things you did before your operation. In fact the formation of
your stoma may relieve symptoms and you may be able to do more. However, other
effects of your cancer and your general health may limit your activities.
During the first few weeks after your
operation don't overdo things. Don't do energetic activities such as shopping,
lifting heavy items, using a vacuum cleaner or gardening for at least six weeks.
Accept offers of help from family and friends. Try to take some gentle exercise each day and
increase this gradually, for example walking. Take care not to overtire yourself
and make sure you get enough rest. If you used to play sports regularly, you
shouldn't start again for at least six weeks. Ask your doctor or stoma care
nurse what you can and can't do.
If you were working before your operation, you
will probably be able to return after six or eight weeks. You may choose to work
part-time at first. If you're not sure about when you can return, perhaps
because of the type of job you do, check with your doctor. After any big operation it takes a while for
your concentration and reflexes to return as normal. Don't start driving again
without checking with your doctor that it's all right to do so.
You should be able to go on holiday as before,
including travelling abroad. Remember to take extra supplies of your appliances
in case you develop "holiday tummy". Always carry supplies in your hand luggage
in case of emergency.
What about eating and drinking?
You should be able to eat a wide variety of
foods although you may find that some foods upset you. Most people do make some
changes to their diet.
Your cancer, previous treatment or the reasons
why you needed a stoma may mean you have to follow a special diet. You will be
given advice as necessary.
There is no reason why you shouldn't drink
alcohol in moderation. However some people choose to avoid beer and other
carbonated (fizzy) drinks because these can cause wind.
If you have any problems or questions about
diet, speak to your stoma care nurse or ask to see the dietician.
What about sex?
Your general health, the stress of your
illness or the after effects of your operation may affect your ability to have
intercourse. If you have questions about his, speak to your stoma care nurse. You may resume sexual activity about six weeks
after your operation, if you wish to. Many people find their libido (sex drive)
decreases. If you do lose interest in sex, don't worry - this isn't unusual.
You may be more tired than usual. If this is a
problem, you may want to set aside time for physical intimacy after a period of
rest. Following your operation you may need to try
different sexual positions until you find one which is comfortable for both of
you. Loss of confidence and a change in the way you
see yourself may affect your sexual relationship. Again, this isn't unusual -
you may find it helps to talk to your partner about your feelings.
If you have had your rectum removed the
tissues nearby may be affected. You may find it difficult to have intercourse.
For men:
You may have difficulty gaining or maintaining an erection. This can be
embarrassing and difficult to discuss such a personal subject or try to ignore
the problem. However, your doctor or stoma care nurse is used to discussing
these problems and even if they are unable to help you themselves, they can
refer you to someone who can. Your partner can also be present, if you wish.
For women:
Your vagina may be scarred and narrowed. This may make intercourse difficult and
painful. You may find it embarrassing to talk about such a personal subject.
However, your doctor or stoma care nurse is used to discussing these problems
and even if they are unable to help you themselves, they can refer you to
someone who can. Your partner can also be present, if you wish.
Remember enjoyable sex needn't depend on
intercourse alone. There are other ways of showing love and sharing pleasure.
USEFUL INFORMATION POINTS
 British
Colostomy Association
15 Station Road
Reading
RG1 1LG
Tel: 0033 173 439 1537
WEBSITE
An information and advisory service. Emotional support on a personal and
confidential basis. Free leaflets and a list of local contacts.
BACK |
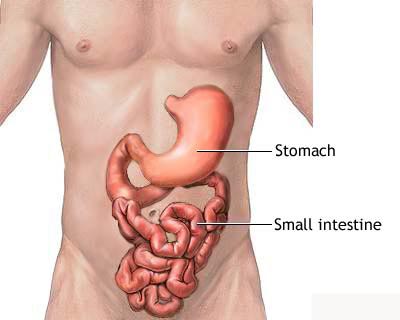 The
small intestine is the portion of the digestive system most responsible for
absorption of nutrients from food into the bloodstream. The pyloric sphincter
governs the passage of partly digested food from the stomach into the duodenum.
This short first portion of the small intestine is followed by the jejunum and
the ileum. The ileocecal valve of the ileum passes digested material into the
large intestine
The
small intestine is the portion of the digestive system most responsible for
absorption of nutrients from food into the bloodstream. The pyloric sphincter
governs the passage of partly digested food from the stomach into the duodenum.
This short first portion of the small intestine is followed by the jejunum and
the ileum. The ileocecal valve of the ileum passes digested material into the
large intestine