Cervical Cancer
Cervical cancer is a disease in which malignant (cancer) cells form in the
tissues of the cervix. Human papillomavirus (HPV) infection is the major risk
factor for development of cervical cancer. There are usually no noticeable signs
of early cervical cancer but it can be detected early with yearly check-ups.
Possible signs of cervical cancer include vaginal bleeding and pelvic pain.
Tests that examine the cervix are used to detect and diagnose cervical cancer.
Certain factors affect prognosis (chance of recovery)
and treatment options.
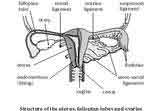
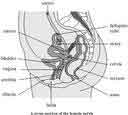
Cervical cancer is a disease in which malignant cells form in the tissues of
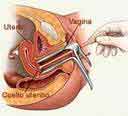
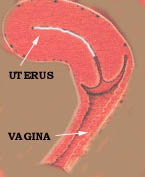
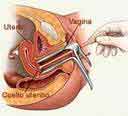
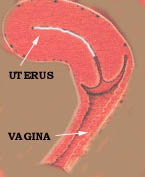
the cervix. The cervix is the lower, narrow end of the uterus (the hollow,
pear-shaped organ where a foetus grows). The cervix leads from the uterus to the
vagina (birth canal). Cervical cancer usually develops slowly over time. Before
cancer appears in the cervix, the cells of the cervix go through changes known
as dysplasia, in which cells that are not normal begin to appear in the cervical
tissue. Later, cancer cells start to grow and spread more deeply into the cervix
and to surrounding areas.
Human papillomavirus (HPV) infection is the major risk factor
for development of cervical cancer. Infection of the cervix with human
papillomavirus (HPV) is the most common cause of cervical cancer. Not all women
with HPV infection, however, will develop cervical cancer. Women who do not
regularly have a Pap smear to detect HPV or abnormal cells in the cervix are at
increased risk of cervical cancer.
Other possible risk factors include the following:
-
Giving
birth to many children
-
Having many
sexual partners
-
Having
first sexual intercourse at a young age
-
Smoking
cigarettes
-
A diet
lacking in vitamins A and C
-
Oral
contraceptive use ("the Pill")
-
Weakened immune system
There are usually no noticeable signs of early cervical cancer
but it can be detected early with yearly check-ups. Early cervical cancer may
not cause noticeable signs or symptoms. Women should have yearly check-ups,
including a Pap smear to check for abnormal cells in the cervix. The prognosis
(chance of recovery) is better when the cancer is found early. Possible signs of
cervical cancer include vaginal bleeding and pelvic pain. These and other
symptoms may be caused by cervical cancer or
by other conditions. A doctor should be consulted if any of the following
problems occur:
 Vaginal bleeding. Vaginal bleeding.
Unusual vaginal discharge.
Pelvic pain.
Pain during sexual intercourse.
Tests that examine the cervix are used to detect and diagnose
cervical cancer. The following procedures may be used:
-
Pap smear: A procedure to collect cells from the surface of
the cervix and vagina. A piece of cotton, a brush, or a
small wooden stick is used to gently scrape cells from the
cervix and vagina. The cells are viewed under a microscope
to find out if they are abnormal. This procedure is also
called a Pap test.
-
Colposcopy: A procedure to look inside the vagina and cervix
for abnormal areas. A colposcope (a thin, lighted tube) is
inserted through the vagina into the cervix. Tissue samples
may be taken for biopsy.
-
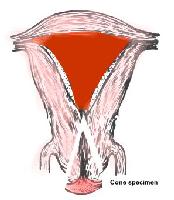
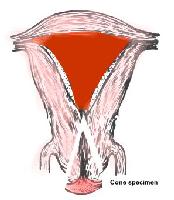
Biopsy: If abnormal cells are found in a Pap smear, the
doctor may do a biopsy. A sample of tissue is cut from the
cervix and viewed under a microscope. A biopsy that removes
only a small amount of tissue is usually done in the
doctor’s office. A woman may need to go to a hospital for a
cervical cone biopsy (removal of a larger, cone-shaped
sample of cervical tissue).
-
Pelvic exam: An exam of the vagina, cervix, uterus,
fallopian tubes, ovaries, and rectum. The doctor or nurse
inserts one or two lubricated, gloved fingers of one hand
into the vagina and the other hand is placed over the lower
abdomen to feel the size, shape, and position of the uterus
and ovaries. A speculum is also inserted into the vagina and
the doctor or nurse looks at the vagina and cervix for signs
of disease. A Pap test or Pap smear of the cervix is usually
done. The doctor or nurse also inserts a lubricated, gloved
finger into the rectum to feel for lumps or abnormal areas.
-
Endocervical curettage: A procedure to collect cells or
tissue from the cervical canal using a curette (spoon-shaped
instrument). Tissue samples may be taken for biopsy. This
procedure is sometimes done at the same time as a
colposcopy.
Certain factors affect prognosis (chance of recovery) and treatment options. The prognosis depends on the following:
-
The stage of the cancer (whether it
affects part of the cervix, involves the whole cervix, or has spread to the
lymph nodes or other places in the body)
-
The type of
cervical cancer
-
The size of
the tumour
Treatment options depend on the following:
Treatment of cervical cancer during pregnancy depends on the stage of the cancer
and the stage of the pregnancy. For cervical cancer found early or for cancer
found during the last trimester of pregnancy, treatment may be delayed until
after the baby is born.
Stages of Cervical Cancer
After cervical cancer has been diagnosed, tests are done to find out if cancer
cells have spread within
the cervix or to other parts of the body. The following stages are used for
cervical cancer:
Stage 0 (Carcinoma in Situ)
Stage I
Stage II
Stage III
Stage IV
After cervical cancer has been diagnosed, tests are done to find out if cancer
cells have spread within the cervix or to other parts of the body. The process
used to find out if cancer has spread within the
cervix or to other parts of the body is called staging. The information gathered
from the staging process determines the stage of the disease. It is important to
know the stage in order to plan treatment. The following tests and procedures
may be used in the staging process:
-
Chest x-ray: An x-ray of the organs and bones inside the
chest. An x-ray is a type of energy beam that can go through
the body and onto film, making a picture of areas inside the
body.
-
CT scan (CAT scan): A procedure that makes a series of
detailed pictures of areas inside the body, taken from
different angles. The pictures are made by a computer linked
to an x-ray machine. A dye may be injected into a vein or
swallowed to help the organs or tissues show up more
clearly. This procedure is also called computed tomography,
computerized tomography, or computerized axial tomography.
-
Lymphangiogram: A procedure used to x-ray the lymph system.
A dye is injected into the lymph vessels in the feet. The
dye travels upward through the lymph nodes and lymph
vessels, and x-rays are taken to see if there are any
blockages. This test helps find out whether cancer has
spread to the lymph nodes.
-
Pre-treatment surgical staging: Surgery (an operation) is
done to find out if the cancer has spread within the cervix
or to other parts of the body. In some cases, the cervical
cancer can be removed at the same time. Pre-treatment
surgical staging is usually done only as part of a clinical
trial.
-
Ultrasound: A procedure in which high-energy sound waves
(ultrasound) are bounced off internal tissues or organs and
make echoes. The echoes form a picture of body tissues
called a sonogram.
-
MRI (magnetic resonance imaging): A procedure that uses a
magnet, radio waves, and a computer to make a series of
detailed pictures of areas inside the body. This procedure
is also called nuclear magnetic resonance imaging (NMRI).
The results of these tests are viewed together with the results
of the original tumour biopsy to determine the cervical cancer stage.
The following stages are used for cervical cancer:
Stage 0 (Carcinoma in Situ)
In stage 0, cancer is found in the first layer of cells lining the cervix only
and has not invaded the deeper tissues of the cervix. Stage 0 is also called
carcinoma in situ.
Stage I:In stage I, cancer is found in the cervix only. Stage I
is divided into stages IA and IB, based on the amount of cancer that is found.
Stage IA: A very small amount of cancer that can only be seen
with a microscope is found in the tissues of the cervix. The cancer is not
deeper than 5 millimetres (less than ¼ inch) and not wider than 7 millimetres
(about ¼ inch).
Stage IB: In stage IB, cancer is still within the cervix and
either can only be seen with a microscope and is deeper than 5 millimetre (less
than ¼ inch) or wider than 7 millimetres (about ¼ inch) or can be seen without a
microscope and may be larger than 4 centimetres (about 1 ½ inches).
Stage II: In stage II, cancer has spread beyond the cervix but
not to the pelvic wall (the tissues that line the part of the body between the
hips). Stage II is divided into stages IIA and IIB, based on how far the cancer
has spread.
Stage IIA: Cancer has spread beyond the cervix to the upper two
thirds of the vagina but not to tissues around the uterus.
Stage IIB: Cancer has spread beyond the cervix to the upper two thirds of the
vagina and to the tissues around the uterus.
Stage III: In stage III, cancer has spread to the lower third of the vagina and
may have spread to the pelvic wall and nearby lymph nodes. Stage III is divided
into stages IIIA and IIIB, based on how far the cancer has spread.
Stage IIIA: Cancer has spread to the lower third of the vagina
but not to the pelvic wall.
Stage IIIB: Cancer has spread to the pelvic wall and/or the
tumour has become large enough to block the ureters (the tubes that connect the
kidneys to the bladder). This blockage can cause the kidneys to enlarge or stop
working. Cancer cells may also have spread to lymph nodes in the pelvis.
Stage IV: In stage IV, cancer has spread to the bladder, rectum or other parts
of the body. Stage IV is divided into stages IVA and IVB, based on where the
cancer is found.
Stage IVA: Cancer has spread to the bladder or rectal wall and may have spread
to lymph nodes in the pelvis.
Stage IVB: Cancer has spread beyond the pelvis and pelvic lymph nodes to other
places in the body, such as the abdomen, liver, intestinal tract, or lungs.
There are different types of treatment for patients with cervical cancer. Three
types of standard treatment are used:
There are different types of treatment for patients with cervical cancer.
Different types of treatment are available for patients with cervical cancer.
Some treatments are standard (the currently used treatment), and some are being
tested in clinical trials. Before starting treatment, patients may want to think
about taking part in a clinical trial. A treatment clinical trial is a research
study meant to help improve current treatments or obtain information on new
treatments for patients with cancer. When clinical trials show that a new
treatment is better than the “standard” treatment, the new treatment may become
the standard treatment. Three types of standard treatment are used:
Surgery (removing the cancer in an operation) is sometimes used
to treat cervical cancer. The following surgical procedures may be used:
-
Conization: A procedure to remove a cone-shaped piece of
tissue from the cervix and cervical canal. A pathologist views the tissue
under a microscope to look for cancer cells. Conization may be used to
diagnose or treat a cervical condition. This procedure is also called a cone
biopsy.
-
Hysterectomy: A surgical procedure to remove the uterus and
cervix. If the uterus and cervix are taken out through the vagina, the
operation is called a vaginal hysterectomy. If the uterus and cervix are taken
out through a large incision in the abdomen, the operation is called a total
abdominal hysterectomy. If the uterus and cervix are taken out through a small
incision in the abdomen using a laparoscope, the operation is called a total
laparoscopic hysterectomy.
-
Bilateral salpingo-oophorectomy: A surgical procedure to
remove both ovaries and both fallopian tubes.
-
Radical hysterectomy: A surgical procedure to remove the
uterus, cervix, and part of the vagina. The ovaries or lymph nodes may also be
removed.
-
Pelvic exenteration: A surgical procedure to remove the lower
colon, rectum, and bladder. In women, the cervix, vagina, ovaries, and nearby
lymph nodes are also removed. Artificial openings (stoma) are made for urine
and stool to flow from the body to a collection bag. Plastic surgery may be
needed to make an artificial vagina after this operation.
-
Cryosurgery: A treatment that uses an instrument to freeze and
destroy abnormal tissue, such as carcinoma in situ. This type of treatment is
also called cryotherapy. Laser surgery: A cancer treatment that uses a laser beam (a
narrow beam of intense light) as a knife to remove cancer. Loop
electrosurgical excision procedure (LEEP): A treatment that uses electrical
current passed through a thin wire loop as a knife to remove abnormal tissue
or cancer.
-
Radiation therapy is a cancer treatment that uses high-energy
x-rays or other types of radiation to kill cancer cells. There are two types
of radiation therapy. External radiation therapy
uses a machine outside the body to send radiation toward the cancer. Internal
radiation therapy uses a radioactive substance sealed in needles, seeds,
wires, or catheters that are placed directly into or near the cancer. The way
the radiation therapy is given depends on the type and stage of
the cancer being treated.
-
Chemotherapy is a cancer treatment that uses drugs to stop the
growth of cancer cells, either by killing the cells or by stopping the cells
from dividing. When chemotherapy is taken by mouth or injected into a vein or
muscle, the drugs enter the bloodstream and can reach cancer cells throughout
the body (systemic chemotherapy). When chemotherapy is placed directly
into the spinal column, a body cavity such as the abdomen, or an organ, the
drugs mainly affect cancer cells in those areas. The way the chemotherapy is
given depends on the type and stage of the cancer being treated.
Other types of treatment are being tested in clinical trials.
BACK
|
|
Endometrial cancer originates in the endometrial lining of the uterus. It is the
most common gynaecological malignancy (cancer originating in female reproductive
organs). The disease normally occurs in postmenopausal women, the average
age at diagnosis being about 60 years.
 Endometrial cancer is considered an oestrogen-dependent
disease. Oestrogen is a hormone that is secreted by the ovaries. It plays an
important role in the development of the female reproductive system and is
largely responsible for the physiologic changes that occur during menstruation,
puberty, and pregnancy. Progesterone is another hormone secreted by the ovaries
that plays an important role. Normally, both oestrogen and progesterone are
secreted in certain proportions. Chronic exposure to oestrogen, without the
accompanying balancing effects of progesterone, is considered the major risk
factor for endometrial cancer and may play a causal role in the development of
the disease. Endometrial cancer is considered an oestrogen-dependent
disease. Oestrogen is a hormone that is secreted by the ovaries. It plays an
important role in the development of the female reproductive system and is
largely responsible for the physiologic changes that occur during menstruation,
puberty, and pregnancy. Progesterone is another hormone secreted by the ovaries
that plays an important role. Normally, both oestrogen and progesterone are
secreted in certain proportions. Chronic exposure to oestrogen, without the
accompanying balancing effects of progesterone, is considered the major risk
factor for endometrial cancer and may play a causal role in the development of
the disease.
Benign uterine tumours, known as fibroids, usually are
asymptomatic and do not require treatment. If fibroids cause bleeding or pain,
they may be surgically removed. Cancerous (malignant) uterine tumours spread to
other tissues and organs if left untreated. Endometrial cancer refers
specifically to tumours that originate in the endometrial lining of the uterus.
If the tumour originates in the deeper, muscular walls of the uterus, it is
called uterine sarcoma. About 90% of all uterine cancers are endometrial.
A precancerous condition called endometrial hyperplasia, or
adenomatous hyperplasiam, may cause irregular uterine bleeding. This condition
can be mild, moderate, or severe. Severe hyperplasia is considered carcinoma in
situ, the earliest detectable stage of endometrial cancer.
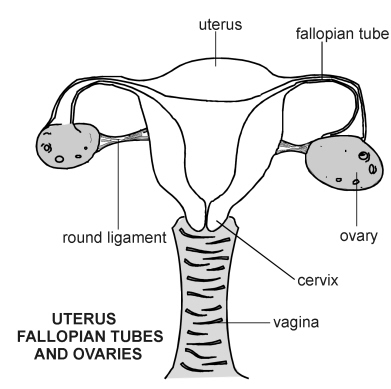
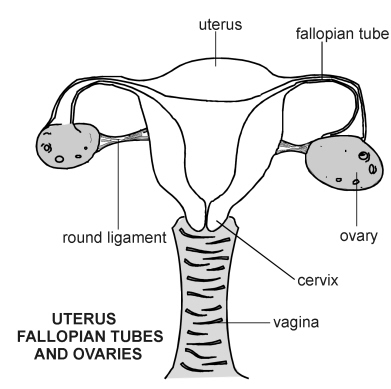
Anatomy of the uterus and endometrium
The uterus (womb) is a muscular, upside-down, pear-shaped organ that is located
in a woman's pelvis behind the bladder and in front of the rectum. The top,
wider part of the uterus is called the fundus (body), and the bottom, narrow
part is the cervix. The fundus has very thick, muscular walls that are lined
with a mucous surface called the endometrium.
Two uterine tubes, the fallopian tubes or oviducts, lead from
either side of the upper part of the uterus to the ovaries. The ovaries are
paired organs, one on each side of the pelvis. Ova (eggs) are transported from
the ovaries to the uterus via the fallopian tubes.
All of the parts of the female genital tract, from the ovaries
to the vagina, are held together by various types of connective tissue. For
example, there is a thin, delicate sheet of lining called the peritoneum that
covers the uterus and extends over the bladder and rectum, keeping the uterus
snug between the latter two organs. But, despite all the well-connected organs,
the female genital tract is more mobile and plastic than any other part of a
woman's body. The ovaries rupture monthly, the uterus sheds countless cells
during menstruation, and the changes that a woman's uterus undergo during
pregnancy are the most dramatic changes that any human organ experiences without
suffering damage. A woman's reproductive system is incredibly responsive to
hormonal changes in its environment. The endometrium is no exception. It is very
sensitive to hormonal changes, and it is believed that endometrial cancer may be
caused by an imbalance in its hormonal environment.
The endometrium contains several layers of cells that vary in
appearance and amount as a woman's menstrual cycle changes. It is full of
glandular cells and blood vessels. Nearly all of the cells are responsive to the
hormonal changes that the uterus regularly experiences. Certain cells undergo
what is called hyperplasia, increased cell division, in response to oestrogen.
It is this cell-growing response to oestrogen that leads many researchers to
believe that oestrogen likely plays a causal role in the development of
endometrial cancer.
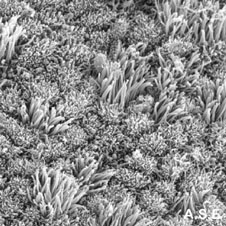
 The uterus has a flat, inner surface and is covered with tall,
columnar epithelial cells. There are pits in the surface that lead down into
uterine glands. The columnar cells, the pits, and the connective tissue and
blood vessels that surround the glands are all part of the endometrium. The
endometrium undergoes dramatic changes during a woman's menstrual cycle. During
the luteal phase, for example, the two-week period just before a woman bleeds,
the endometrium is thick, its epithelial cells are enlarged, the glands bulging,
and the arteries swollen. At menstruation, the arteries break, the epithelial
cells die, and the endometrium, in effect, sheds. Following menstruation, during
the follicular phase, the endometrium regenerates. The changing thickness of the
endometrium is highly dependent on the secretion of oestrogen and progesterone.
Oestrogen causes cellular growth and is an important component of the
rebuilding, follicular phase of the menstrual cycle. Progesterone is secreted
during the later, thick-walled luteal phase, and it balances out the effects of
the oestrogen. Abnormal growth of endometrial cells (whether cancerous or not)
and endometrial cancer are believed to be due to chronic exposure to too much
oestrogen without the balancing effect of progesterone. The uterus has a flat, inner surface and is covered with tall,
columnar epithelial cells. There are pits in the surface that lead down into
uterine glands. The columnar cells, the pits, and the connective tissue and
blood vessels that surround the glands are all part of the endometrium. The
endometrium undergoes dramatic changes during a woman's menstrual cycle. During
the luteal phase, for example, the two-week period just before a woman bleeds,
the endometrium is thick, its epithelial cells are enlarged, the glands bulging,
and the arteries swollen. At menstruation, the arteries break, the epithelial
cells die, and the endometrium, in effect, sheds. Following menstruation, during
the follicular phase, the endometrium regenerates. The changing thickness of the
endometrium is highly dependent on the secretion of oestrogen and progesterone.
Oestrogen causes cellular growth and is an important component of the
rebuilding, follicular phase of the menstrual cycle. Progesterone is secreted
during the later, thick-walled luteal phase, and it balances out the effects of
the oestrogen. Abnormal growth of endometrial cells (whether cancerous or not)
and endometrial cancer are believed to be due to chronic exposure to too much
oestrogen without the balancing effect of progesterone.
Treatment
The treatment of endometrial cancer depends on many factors, including a
patient's general health, age, and stage of the disease. In the early stages, endometrial cancer is usually treated with
surgery and/or radiation. In the later stages, it
is usually treated with hormone therapy. There are
numerous treatment options for patients.
Surgery
The typical surgery is bilateral salpingo-oophorectomy, the removal of the
ovaries and fallopian tubes, as well as a complete, radical hysterectomy. A
radical hysterectomy involves removing the uterus, the tissues surrounding the
uterus, and the upper third of the vagina. A hysterectomy can be either
abdominal or vaginal. In an abdominal hysterectomy, the surgeon makes an
incision in the front of the abdomen and removes the uterus. In a vaginal
hysterectomy, the uterus is removed through the vagina. Because endometrial
cancer originates in the uterine body, a hysterectomy should be sufficient, but
the ovaries are removed as well because they are the most common sites of
undetected metastasis. Also, most women who undergo the surgery are
postmenopausal, and their ovaries are no longer providing the hormonal function
that is so important before menopause. During an abdominal hysterectomy, the
lymph nodes are also almost always sampled (a pelvic lymph node dissection) to
detect any spread of cancer to the lymph nodes.
Until recently, if a vaginal hysterectomy was used to remove the uterus,
there was no way to get a sample of lymph node tissue. Now, however, there is a
new surgical technique called laparascopic lymph node sampling that many
surgeons are beginning to use that allows for sampling the lymph nodes even when
the abdomen is not cut open for an abdominal hysterectomy. Thus women can opt
for a vaginal hysterectomy and still have their lymph nodes examined. The new
method involves inserting a tube through a very small opening in the abdomen.
The vaginal hysterectomy combined with the laparascopy are much less invasive
and require less recovery time than an abdominal hysterectomy.
Although the primary treatment for any stage endometrial cancer involves a
radical hysterectomy, according to the National Cancer Institute, early stage I
cancers may not require a radical hysterectomy. A simple hysterectomy,which
involves removal of the uterus but not the surrounding tissues or upper third of
the vagina, may be sufficient. It is important that you discuss with your
surgeon the different options and why she or he thinks one procedure is more
appropriate than another.
Radiation
There are two types of radiotherapy commonly used to treat various stages and
grades of endometrial cancer: external-beam
pelvic radiation and
intra-cavitary
irradiation.
External beam pelvic radiation
Radiotherapy was first used to treat uterine cancer around the turn of the
century, very shortly after Marie Curie's discovery of radium. For many decades,
radiation therapy was used as a standard pre-surgical treatment, but it is no
longer done preoperatively because it prevents accurate surgical staging. It is
standard to reserve the use of radiotherapy until an initial hysterectomy, at
least, has been performed. Even following a hysterectomy and bilateral
salpingo-oophorectomy, however, the effectiveness of adjuvant radiation therapy
(therapy used in addition to surgery) is controversial. Although regional pelvic
radiation has proven to decrease pelvic recurrences, it does not necessarily
improve the survival rate. It is likely most beneficial for patients with
tumours that are confined to the pelvis and that have features that increase the
likelihood of recurrence (stages IC to IIIC). The potential benefits of
radiation should be weighed against the risks, such as a history of pelvic
infections or severe diabetes mellitus.
Postoperative vaginal irradiation (brachytherapy)
In addition to pelvic radiation, postoperative vaginal irradiation is often used
to prevent vaginal cuff recurrences (the vaginal cuff is the upper third of the
vagina). Vaginal cuff recurrences are common for certain types of tumours. This
type of therapy involves inserting small metal cylinders, or some other type of
applicator, through the vagina, where it releases a radioactive substance over
the course of two or three days.
Hormonal therapy
Hormones, particularly progesterone, can be used to treat metastatic endometrial
cancer, but their effectiveness is not very great. Studies indicate that less
than 20% of patients who are treated with hormones respond to the treatment.
Chemotherapy
Studies have not yet produced clear results on the effectiveness of chemotherapy
to treat endometrial cancer. Chemotherapy is potentially most useful for cancers
that have spread to distant parts of the body.
Treatment by stage
Stages I and II
Hysterectomy and bilateral salpingo-oophorectomy plus radiation, depending on
the grade of the tumour and whether it has invaded the myometrium.
Stage IA, grade 1 or 2 tumour
Usually there is a low risk of disease recurrence, therefore radiation therapy
is not used. Treatment is surgery only.
Stage IA, grade 3 tumour; all stage II tumours
There is an intermediate risk for disease recurrence in these patients, although
it is not clear that postoperative radiation therapy improves survival. It does,
however, decrease the risk of local relapse. Following surgery, it is important
that patients be given the opportunity to participate in clinical, postoperative
radiation therapy trials. Either vaginal cuff radiation (internal radiation of
the upper third of the vagina) or pelvic radiation should be considered.
Stages III and IVA (all grade tumours)
Following surgery, vaginal cuff radiotherapy with or without pelvic or whole
abdominal radiation may increase a woman's chances of survival. Progesterone is
used for metastatic endometrial cancer.
Stage IVB
This group of women have distant spread of the disease at the time of diagnosis.
The chance of cure in this group is, unfortunately, low. If possible, patients
can participate in a clinical trial. If not possible, or if they choose not to
participate, palliative (pain-relieving) therapy should be considered.
Palliation of symptoms can include hormones, chemotherapy, or radiation.
Recurrent disease
Recurrence is more likely in women with advanced disease and in those whose
tumour had certain high-risk features. Usually recurrence happens within three
years of the original diagnosis. Hormone therapy can be used to treat recurrent
disease, although its effectiveness does not appear to be that great. The use of
various combinations of hormones are currently being evaluated. The use of
chemotherapy to treat recurrent disease is also currently being evaluated. If a
woman was originally treated only with surgery and no radiation, if the cancer
recurs, either external-beam pelvic or intracavitary radiation can be used as
therapy. In the case of radiation, the prognosis depends on many features such
as the size and extent of the tumour and the time to recurrence.
BACK
|
Ovarian Cancers
Women who have a family
history of ovarian cancer are at an increased risk of developing ovarian cancer. Women who have one first-degree relative (mother, daughter, or
sister) with ovarian cancer are at an increased risk of developing ovarian
cancer. This risk is higher in women who have one first-degree relative and one
second-degree relative (grandmother or aunt) with ovarian cancer. This risk is
even higher in women who have two or more first-degree relatives with ovarian
cancer. Some ovarian cancers are caused by inherited gene mutations (changes).
Women who have one first-degree relative (mother, daughter, or
sister) with ovarian cancer are at an increased risk of developing ovarian
cancer. This risk is higher in women who have one first-degree relative and one
second-degree relative (grandmother or aunt) with ovarian cancer. This risk is
even higher in women who have two or more first-degree relatives with ovarian
cancer. Some ovarian cancers are caused by inherited gene mutations (changes).Ovarian cancer is a disease
produced by the rapid growth and division of cells within one or both
ovaries—reproductive glands in which the ova, or eggs, and the female sex
hormones are made. The ovaries contain cells that, under normal circumstances,
reproduce to maintain tissue health. When growth control is lost and cells
divide too much and too fast, a cellular mass is formed. If the tumour is
confined to a few cell layers, for example, surface cells,
 and it does not
invade surrounding tissues or organs, it is considered benign. If the tumour
spreads to surrounding tissues or organs, it is considered malignant, or
cancerous. When cancerous cells break away from the original tumour, travel
through the blood or lymphatic vessels, and grow within other parts of the body,
the process is known as metastasis and it does not
invade surrounding tissues or organs, it is considered benign. If the tumour
spreads to surrounding tissues or organs, it is considered malignant, or
cancerous. When cancerous cells break away from the original tumour, travel
through the blood or lymphatic vessels, and grow within other parts of the body,
the process is known as metastasis
Many kinds of tumours can form in the ovaries. In fact, there are over 30
known histopathologic, or diseased tissue, types. Experts group ovarian cancers
within three major categories, according to the type of cells from which they
were formed. 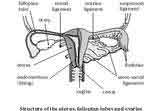
- Epithelial cancers, which are the most common ovarian cancers, arise from
cells lining or covering the ovaries.
- Germ cell cancers start from germ cells (cells that are destined to form
eggs) within the ovaries.
- Sex cord, stromal cell cancers, begin in the cells that hold the ovaries
together and produce female hormones.
Incidence and Prevalence
Ovarian cancer is a disease that principally affects middle and upper-class
women in industrialized nations. It is uncommon in underdeveloped countries,
perhaps because of different dietary factors in these regions
It is estimated that approximately 30,000 new cases of ovarian cancer will be
diagnosed this year, with 15,000 women dying from this disease. Ovarian cancer
most frequently appears in women who are older than 60 (about 50% of patients
are over age 65), although it may occur in younger women who have a family
history of the disease. Ovarian cancer is responsible for 5% of all cancer
deaths among women.
There are marked differences in survival among patients with ovarian cancer,
depending on factors such as age, cancer stage, and tissue type. Younger
patients tend to fare better in all stages than do older patients, whereas race
does not play a factor, as it does in other cancers. Survival rates are similar
in black and white women.
Ovarian Anatomy
The ovaries are female reproductive organs that are akin to the testes in men.
They produce the ova (eggs) that, when fertilized, will develop into a foetus;
they also generate the female sex hormones oestrogen and progesterone. There are
two ovaries, each of which is located within the pelvic region beside the uterus
(womb).
Ovarian Structure
The ovaries are oval-shaped and are approximately 1 ½ inches in length. They are
pinkish-grey in colour and have an uneven surface. The ovaries are connected to
the uterus by the fallopian tubes, or oviducts, which carry the eggs into the
uterine cavity. Each ovary contains numerous Graafian follicles, egg-containing
tubes that grow and develop between puberty, sexual maturation, and menopause,
when the monthly menstrual cycle stops. When a woman is fertile, each month a
Graafian follicle travels to the surface of the ovary, bursts, and releases an
egg and its fluid contents into a fallopian tube.
The Graafian follicles are fixed in a network of supporting tissue (stroma)
and blood vessels. They are covered by a clear, smooth, plasma-like membrane
that develops from the peritoneum - lining of the abdominal cavity. Also within
the ovaries are small numbers of corpus lutea - the remains of Graafian
follicles that have released an egg and are in the process of being reabsorbed
by ovarian tissue. Each month the corpus luteum (the scar tissue of a Graafian
follicle) is responsible for the production of progesterone. Progesterone is the
pregnancy hormone that readies the lining of the uterus for the arrival of a
fertilized egg.
Ovarian Function
During the first half of a woman's menstrual cycle - about 2 weeks before
ovulation, an egg is released. The hypothalamus in the brain sends a hormonal
signal to the pituitary gland to release follicle-stimulating hormone (FSH) into
the bloodstream. When the blood-borne FSH reaches the ovaries, it spurs the
Graafian follicles to grow and produce oestrogen. Additional oestrogen is made
by hormone-producing tissue within the stroma. One Graafian follicle in an ovary
begins to outgrow the other follicles while the eostrogen level is increasing.
Meanwhile, once the oestrogen level has peaked, the pituitary gland stops the
output of FSH and begins to release luteinizing hormone (LH). The LH causes the
Graafian follicle to bubble out on the outside of the ovary, burst, and eject
its egg into the fallopian tube. This process of ovulation occurs on or about
the 14th day of the menstrual cycle. The ovulated egg travels through the
fallopian tube for 5 to 7 days, after which it is released into the uterus.
Connective Tissue
The ovaries are held in place by bands of fibrous tissue known as ligaments. The
ligament of the ovary is a rounded cord that extends from the upper uterus to
the lower, inner region of the ovary. The fimbria ovarica are fringe-like
tissues that attach the ovaries to the fallopian tubes. The round ligaments are
two cords, 4 to 5 inches in length, that connect with layers of the broad
ligament (ligament that attaches to each side of the pelvic wall to support the
uterus) in front of and below the fallopian tubes.
Blood Vessels and Nerves
The ovarian arteries, which are offshoots of the abdominal aorta, furnish the
ovaries and fallopian tubes with blood. They enter the ovary via an attached
border, or hilus. The ovarian veins parallel the route of the arteries, forming
a tangled network in the broad ligament known as the pampiniform plexus.
The nerves that supply the ovaries are branches of the inferior hypogastric
nerve, the pelvic plexus (network), the ovarian plexus, and uterine nerves
within the fallopian tubes.
BACK
|
Sarcoma of the uterus
Sarcoma of the uterus, a very rare kind of cancer in women, is a disease
in which cancer cells start growing in the muscles or other supporting
tissues of the uterus. The uterus is the hollow, pear-shaped organ where a
baby grows. Sarcoma of the uterus is different from cancer of the
endometrium, a disease in which cancer cells start growing in the lining of
the uterus.
Women who have received therapy with high-dose x-rays (external-beam
radiation therapy) to their pelvis are at a higher risk to develop sarcoma
of the uterus. These x-rays are sometimes given to women to stop bleeding
from the uterus.
A doctor should be seen if there is bleeding after menopause (the time
when a woman no longer has menstrual periods) or bleeding that is not part
of menstrual periods.
Sarcoma of the uterus usually begins after menopause. If there are signs of cancer, a doctor will do certain tests to check for
cancer, usually beginning with an internal (pelvic) examination. During the
examination, the doctor will feel for any lumps or changes in the shapes of
the pelvic organs. The doctor may then do a Pap test, using a piece of
cotton, a small wooden stick, or brush to gently scrape the outside of the
cervix (the opening of the uterus) and the vagina to pick up cells. Because
sarcoma of the uterus begins inside, this cancer will not usually show up on
the Pap test. The doctor may also do a dilation and curettage (D & C) by
stretching the cervix and inserting a small, spoon-shaped instrument into
the uterus to remove pieces of the lining of the uterus. This tissue is then
checked under a microscope for cancer cells.
The prognosis (chance of recovery) and choice of treatment depend on the
stage of the sarcoma (whether it is just in the uterus or has spread to
other places), how fast the tumour cells are growing, and the patient’s
general state of health.
|
Stages of sarcoma of the uterusOnce sarcoma of the uterus has been found, more tests will be done to find
out if the cancer has spread from the uterus to other parts of the body
(staging). A doctor needs to know the stage of the disease to plan treatment.
The following stages are used for sarcoma of the uterus:
Stage I
Cancer is found only in the main part of the uterus (it is not found in the
cervix).
Stage II
Cancer cells have spread to the cervix.
Stage III
Cancer cells have spread outside the uterus but have not spread outside the
pelvis.
Stage IV
Cancer cells have spread beyond the pelvis, to other body parts, or into the
lining of the bladder (the sac that holds urine) or rectum.
Recurrent
Recurrent disease means that the cancer has come back (recurred) after it has
been treated.
How sarcoma of the uterus is treated
There are treatments for all patients with sarcoma of the uterus. Four kinds
of treatment are used:
- Surgery (taking out the cancer in an operation).
- Radiation therapy (using high-dose x-rays or other high-energy
rays to kill cancer cells and shrink tumors).
- Chemotherapy (using drugs to kill cancer cells).
- Hormone therapy (using female hormones to kill cancer cells).
Surgery is the most common treatment of sarcoma of the uterus. A doctor may
take out the cancer in an operation to remove the uterus, fallopian tubes and
the ovaries, along with some lymph nodes in the pelvis and around the aorta (the
main vessel in which blood passes away from the heart). The operation is called
a total abdominal hysterectomy, bilateral salpingo-oophorectomy, and
lymphadenectomy. (The lymph nodes are small bean-shaped structures that are
found throughout the body. They produce and store infection-fighting cells, but
may contain cancer cells.)
Radiation therapy uses x-rays or other high-energy rays to kill cancer cells
and shrink tumours. Radiation therapy for sarcoma of the uterus usually comes
from a machine outside the body (external radiation). Radiation may be used
alone or in addition to surgery.
Chemotherapy uses drugs to kill cancer cells. Chemotherapy may be taken by
pill, or it may be put into the body by a needle in a vein or a muscle.
Chemotherapy is called a systemic treatment because the drugs enter the
bloodstream, travel through the body, and can kill cancer cells outside the
uterus.
Hormone therapy uses female hormones, usually taken by pill, to kill cancer
cells.
Treatment by stage
Treatment of sarcoma of the uterus depends on the stage and cell type of the
disease, and the patient’s age and overall condition. Standard treatment may be considered because of its effectiveness in patients
in past studies, or participation in a clinical trial may be considered. Not all
patients are cured with standard therapy and some standard treatments may have
more side effects than are desired. For these reasons, clinical trials are
designed to find better ways to treat cancer patients and are based on the most
up-to-date information.
Stage I Uterine Sarcoma
Treatment may be one of the following:
- Surgery to remove the uterus, fallopian tubes and the ovaries,
and some of the lymph nodes in the pelvis and abdomen (total abdominal
hysterectomy, bilateral salpingo-oophorectomy, and lymph node dissection)
- Total abdominal hysterectomy, bilateral salpingo-oophorectomy,
and lymph node dissection, followed by radiation therapy to the pelvis.
- Surgery followed by chemotherapy.
- Surgery followed by radiation therapy.
Stage II Uterine Sarcoma
Treatment may be one of the following:
- Surgery to remove the uterus, fallopian tubes and the ovaries,
and some of the lymph nodes in the pelvis and abdomen (total abdominal
hysterectomy, bilateral salpingo-oophorectomy, and lymph node dissection)
- Total abdominal hysterectomy, bilateral salpingo-oophorectomy,
and lymph node dissection, followed by radiation therapy to the pelvis.
- Surgery followed by chemotherapy.
- Surgery followed by radiation therapy.
Stage III Uterine Sarcoma
Treatment may be one of the following:
- Surgery to remove the uterus, fallopian tubes and the ovaries,
and some of the lymph nodes in the pelvis and abdomen (total abdominal
hysterectomy bilateral salpingo-oophorectomy, and lymph node dissection).
Doctors will also try to remove as much of the cancer that has spread to
nearby tissues as possible.
- Total abdominal hysterectomy, bilateral salpingo-oophorectomy,
and lymph node dissection, followed by radiation therapy to the pelvis.
- Surgery followed by chemotherapy.
Stage IV Uterine Sarcoma
Treatment will usually be a clinical trial using chemotherapy.
Recurrent Uterine Sarcoma
If the cancer has come back (recurred), treatment may be one of the
following:
- Clinical trials of chemotherapy or hormone therapy.
- External radiation therapy to relieve symptoms such as pain,
nausea, or abnormal bowel functions.
BACK
|
| Vaginal Cancer
Cancer of the vagina, a rare kind of cancer in women, is a disease in which
cancer (malignant) cells are found in the tissues of the vagina. The vagina is
the passageway through which fluid passes out of the body during menstrual
periods and through which a woman has babies. It is also called the "birth
canal." The vagina connects the cervix (the opening of the womb or uterus) and
the vulva (the folds of skin around the opening to the vagina).
There are two types of cancer of the vagina: squamous cell cancer (squamous
carcinoma) and adenocarcinoma. Squamous carcinoma is usually found in women
between the ages of 60 and 80. Adenocarcinoma is more often found in women
between the ages of 12 and 30.
Young women whose mothers took DES (diethylstilbestrol) are at risk
of
getting tumours in their vaginas. Some of them get a rare form of cancer called
clear cell adenocarcinoma. The drug DES was given to pregnant women between 1945
and 1970 to keep them from losing their babies (miscarriage).
A doctor should be seen if there are any of the following:
- Bleeding or discharge not related to menstrual periods.
- Difficult or painful urination.
- Pain during intercourse or in the pelvic area.
- Also, there is still a chance of developing vaginal cancer in
women who have had a hysterectomy.
A doctor may use several tests to see if there is cancer. The doctor will
usually begin by giving the patient an internal (pelvic) examination. The doctor
will feel for lumps and will then do a Pap smear. Using a piece of cotton, a
brush, or a small wooden stick, the doctor will gently scrape the outside of the
cervix and vagina in order to pick up cells. Some pressure may be felt, but
usually with no pain.
If cells that are not normal are found, the doctor will need to cut a small
sample of tissue (called a biopsy) out of the vagina and look at it under a
microscope to see if there are any cancer cells. The doctor should look not only
at the vagina, but also at the other organs in the pelvis to see where the
cancer started and where it may have spread. The doctor may take an x-ray of the
chest to make sure the cancer has not spread to the lungs.
The chance of recovery (prognosis) and choice of treatment depend on the
stage of the cancer (whether it is just in the vagina or has spread to other
places) and the patient's general state of health.
Stages of cancer of the vagina
Once cancer of the vagina has been found (diagnosed), more tests will be done
to find out if the cancer has spread from the vagina to other parts of the body
(staging). A doctor needs to know the stage of the disease to plan treatment.
The following stages are used for cancer of the vagina:
Stage 0 or carcinoma in situ
Stage 0 cancer of the vagina is a very early cancer. The cancer is found
inside the vagina only and is in only a few layers of cells.
Stage I
Cancer is found in the vagina, but has not spread outside of it.
Stage II
Cancer has spread to the tissues just outside the vagina, but has not gone to
the bones of the pelvis.
Stage III
Cancer has spread to the bones of the pelvis. Cancer cells may also have
spread to other organs and the lymph nodes in the pelvis. (Lymph nodes are small
bean-shaped structures that are found throughout the body. They produce and
store cells that fight infection.)
Stage IVA
Cancer has spread into the bladder or rectum.
Stage IVB
Cancer has spread to other parts of the body, such as the lungs.
Recurrent
Recurrent disease means that the cancer has come back (recurred) after it has
been treated. It may come back in the vagina or in another place.
How cancer of the vagina is treated
Treatments are available for all patients with cancer of the vagina. There
are three kinds of treatment:
- Surgery (taking out the cancer in an operation).
- Radiation therapy (using high-dose x-rays or other high-energy
rays to kill cancer cells and shrink tumours).
- Chemotherapy (using drugs to kill cancer cells).
Surgery is the most common treatment of all stages of cancer of the vagina. A
doctor may take out the cancer using one of the following:
- Laser surgery uses a
narrow beam of light to kill cancer cells and is useful for stage 0 cancer
- Wide local excision takes out the cancer and some of the
tissue around it. A patient may need to have skin taken from another part of
the body (grafted) to repair the vagina after the cancer has been taken out.
- An operation in which the vagina is removed (vaginectomy) is
sometimes done. When the cancer has spread outside the vagina, vaginectomy may
be combined with surgery to take out the uterus, ovaries, and fallopian
tubes (radical hysterectomy). During these operations, lymph nodes in the
pelvis may also be removed (lymph node dissection)
- If the cancer has spread outside the vagina and the other
female organs, the doctor may take out the lower colon, rectum, or bladder
(depending on where the cancer has spread) along with the cervix, uterus, and
vagina (exenteration)
- A patient may need skin grafts and plastic surgery to make an
artificial vagina after these operations.
Radiation therapy uses x-rays or other high-energy rays to kill cancer cells
and shrink tumours. Radiation may come from a machine outside the body (external
radiation) or from putting materials that produce radiation (radioisotopes)
through thin plastic tubes into the area where the cancer cells are found
(internal radiation). Radiation may be used alone or after surgery.
Chemotherapy uses drugs to kill cancer cells. Chemotherapy may be taken by
pill, or it may be put into the body by a needle in a vein. Chemotherapy is
called a systemic treatment because the drugs enter the bloodstream, travel
through the body, and can kill cancer cells outside the vagina. In treating
vaginal cancer, chemotherapy may also be put directly into the vagina itself,
which is called intra-vaginal chemotherapy.
Stage 0 Vaginal Cancer
Treatment may be one of the following:
- Surgery to remove all or part of the vagina (vaginectomy).
This may be followed by skin grafting to repair damage done to the vagina.
- Internal radiation therapy.
- Laser surgery.
- Intravaginal chemotherapy
Stage I Vaginal Cancer
Treatment of stage I cancer of the vagina depends on whether a patient has
squamous cell cancer or adenocarcinoma.
If squamous cancer is found, treatment may be one of the following:
- Internal radiation therapy with or without external beam
radiation therapy.
- Wide local excision. This may be followed by the rebuilding of
the vagina. Radiation therapy following surgery may also be performed in some
cases.
- Surgery to remove the vagina with or without lymph nodes in
the pelvic area (vaginectomy and lymph node dissection).
If adenocarcinoma is found, treatment may be one of the following:
- Surgery to remove the vagina (vaginectomy) and the uterus,
ovaries, and fallopian tubes (hysterectomy). The lymph nodes in the pelvis are
also removed (lymph node dissection). This may be followed by the rebuilding
of the vagina. Radiation therapy following surgery may also be performed in
some cases.
- Internal radiation therapy with or without external beam
radiation therapy.
- In selected patients, wide local excision and removal of some
of the lymph nodes in the pelvis followed by internal radiation
Stage II Vaginal Cancer
Treatment of stage II cancer of the vagina is the same whether a patient has
squamous cell cancer or adenocarcinoma.
Treatment may be one of the following:
- Combined internal and external radiation therapy.
- Surgery, which may be followed by radiation therapy.
Stage III Vaginal Cancer
Treatment of stage III cancer of the vagina is the same whether a patient has
squamous cell cancer or adenocarcinoma.
Treatment may be one of the following:
- Combined internal and external radiation therapy.
- Surgery may sometimes be combined with radiation therapy.
Stage IVA Vaginal Cancer
Treatment of stage IVA cancer of the vagina is the same whether a patient has
squamous cell cancer or adenocarcinoma.
Treatment may be one of the following:
- Combined internal and external radiation therapy.
- Surgery may sometimes be combined with radiation therapy
Stage IVB Vaginal Cancer
If stage IVB cancer of the vagina is found, treatment may be radiation to
relieve symptoms such as pain, nausea, vomiting, or abnormal bowel function.
Chemotherapy may also be performed. A patient may also choose to participate in
a clinical trial.
Recurrent Vaginal Cancer
If the cancer has come back (recurred) and spread past the female organs, a
doctor may take out the cervix, uterus, lower colon, rectum, or bladder (exenteration),
depending on where the cancer has spread. The doctor may give the patient
radiation therapy or chemotherapy.
A patient may also choose to participate in a clinical trial of chemotherapy
or radiation therapy.
BACK
|
| Cancer of the
Vulva
Cancer of the vulva, a rare kind of cancer in women, is a disease in which
cancer (malignant) cells are found in the vulva. The vulva is the outer part of
a woman’s vagina. The vagina is the passage between the uterus (the hollow,
pear-shaped organ where a baby grows) and the outside of the body. It is also
called the birth canal.

Most women with cancer of the vulva are over age 50. However, it is becoming
more common in women under age 40. Women who have constant itching and changes
in the colour and the way the vulva looks are at a high risk to get cancer of
the vulva. A doctor should be seen if there is bleeding or discharge not related
to menstruation (periods), severe burning/itching or pain in the vulva, or if
the skin of the vulva looks white and feels rough.
If there are symptoms, a doctor may do certain tests to see if there is
cancer, usually beginning by looking at the vulva and feeling for any lumps. The
doctor may then go on to cut out a small piece of tissue (called a biopsy) from
the vulva and look at it under a microscope. A patient will be given some
medicine to numb the area when the biopsy is done. Some pressure may be felt,
but usually with no pain. This test is often done in a doctor’s office.
The chance of recovery (prognosis) and choice of treatment depend on the
stage of the cancer (whether it is just in the vulva or has spread to other
places) and the patient’s general state of health.
Stages of cancer of the vulva
Once cancer of the vulva is diagnosed, more tests will be done to find out if
the cancer has spread from the vulva to other parts of the body (staging). A
doctor needs to know the stage of the disease to plan treatment. The following
stages are used for cancer of the vulva:
Stage 0 or carcinoma in situ
Stage 0 cancer of the vulva is a very early cancer. The cancer is found in
the vulva only and is only in the surface of the skin.
Stage I
Cancer is found only in the vulva and/or the space between the opening of the
rectum and the vagina (perineum). The tumour is 2 centimetres (about 1 inch) or
less in size.
Stage II
Cancer is found in the vulva and/or the space between the opening of the
rectum and the vagina (perineum), and the tumour is larger than 2 centimetres
(larger than 1 inch).
Stage III
Cancer is found in the vulva and/or perineum and has spread to nearby tissues
such as the lower part of the urethra (the tube through which urine passes), the
vagina, the anus (the opening of the rectum), and/or has spread to nearby lymph
nodes. (Lymph nodes are small bean-shaped structures that are found throughout
the body. They produce and store infection-fighting cells.)
Stage IV
Cancer has spread beyond the urethra, vagina, and anus into the lining of the
bladder (the sac that holds urine) and the bowel (intestine); or, it may have
spread to the lymph nodes in the pelvis or to other parts of the body.
Recurrent
Recurrent disease means that the cancer has come back (recurred) after it has
been treated. It may come back in the vulva or another place.
How cancer of the vulva is treated
There are treatments for all patients with cancer of the vulva. Three kinds
of treatment are used:
- Surgery (taking out the cancer in an operation).
- Radiation therapy (using high-dose x-rays or other high-energy
rays to kill cancer cells).
- Chemotherapy (using drugs to kill cancer cells).
Surgery is the most common treatment of cancer of the vulva. A doctor may
take out the cancer using one of the following operations:
- Wide local excision takes
out the cancer and some of the normal tissue around the cancer
- Radical local excision
takes out the cancer and a larger portion of normal tissue around the
cancer. Lymph nodes may also be removed
- Laser surgery uses a
narrow beam of light to remove cancer cells
- Skinning vulvectomy takes
out only the skin of the vulva that contains the cancer
- Simple vulvectomy takes
out the entire vulva, but no lymph nodes
- Partial vulvectomy takes
out less than the entire vulva
- Radical vulvectomy takes
out the entire vulva. The lymph nodes around it are usually removed as well
- If the cancer has spread outside the vulva and the other
female organs, the doctor may take out the lower colon, rectum, or bladder
(depending on where the cancer has spread) along with the cervix, uterus, and
vagina (pelvic exenteration).
A patient may need to have skin from another part of the body added (grafted)
and plastic surgery to make an artificial vulva or vagina after these
operations.
Radiation therapy uses x-rays or other high-energy rays to kill cancer cells
and shrink tumours. Radiation may come from a machine outside the body (external
radiation) or from putting materials that contain radiation through thin plastic
tubes into the area where the cancer cells are found (internal radiation).
Radiation may be used alone or before or after surgery.
Chemotherapy uses drugs to kill cancer cells. Drugs may be given by mouth, or
they may be put into the body by a needle in the vein or muscle. Chemotherapy is
called systemic treatment because the drug enters the bloodstream, travels
through the body, and can kill cancer cells throughout the body.
BACK
HELPLINES
Jo's Trust - Fighting Cervical Cancer
Pamela Morton
Tel:01327 361787
web site
www.jotrust.co.uk email
pamela@jotrust.co.uk
Ovacome
(for all those involved in ovarian cancer, inc. patients, carers, families etc.)
St Bartholomew's Hospital,
West Smithfield,
London EC1A 7BE
Tel 020 7600 5141 (Monday to Friday 9 a.m. to 1 p.m.)
web site
www.ovacome.org.uk
email
ovacome@ovacome.org.uk
Gynae C (for women with any gynae
cancer, their partners, families & friends)
1 Bolingbroke Road,
Swindon,
SN2 2LB
01793 322005
www.communigate.co.uk/wilts/gynaec/index.phtml
email
gynae_c@yahoo.com
Amarant Trust (advice line for
women going through the menopause)
01293 413000 (Monday to Friday 11a.m. to 6 p.m.)
Radical Vulvectomy Support Group
01977 640 243 (highly confidential telephone support)
V.A.C.O. (Vulva Awareness Charity
Organisation)
Tel 0161 747 5911 (highly
confidential telephone support)
email
carol@jones5911.fsnet.co.uk
BACK |


 Women who have one first-degree relative (mother, daughter, or
sister) with ovarian cancer are at an increased risk of developing ovarian
cancer. This risk is higher in women who have one first-degree relative and one
second-degree relative (grandmother or aunt) with ovarian cancer. This risk is
even higher in women who have two or more first-degree relatives with ovarian
cancer. Some ovarian cancers are caused by inherited gene mutations (changes).
Women who have one first-degree relative (mother, daughter, or
sister) with ovarian cancer are at an increased risk of developing ovarian
cancer. This risk is higher in women who have one first-degree relative and one
second-degree relative (grandmother or aunt) with ovarian cancer. This risk is
even higher in women who have two or more first-degree relatives with ovarian
cancer. Some ovarian cancers are caused by inherited gene mutations (changes).
 Vaginal bleeding.
Vaginal bleeding.  Endometrial cancer is considered an oestrogen-dependent
disease. Oestrogen is a hormone that is secreted by the ovaries. It plays an
important role in the development of the female reproductive system and is
largely responsible for the physiologic changes that occur during menstruation,
puberty, and pregnancy. Progesterone is another hormone secreted by the ovaries
that plays an important role. Normally, both oestrogen and progesterone are
secreted in certain proportions. Chronic exposure to oestrogen, without the
accompanying balancing effects of progesterone, is considered the major risk
factor for endometrial cancer and may play a causal role in the development of
the disease.
Endometrial cancer is considered an oestrogen-dependent
disease. Oestrogen is a hormone that is secreted by the ovaries. It plays an
important role in the development of the female reproductive system and is
largely responsible for the physiologic changes that occur during menstruation,
puberty, and pregnancy. Progesterone is another hormone secreted by the ovaries
that plays an important role. Normally, both oestrogen and progesterone are
secreted in certain proportions. Chronic exposure to oestrogen, without the
accompanying balancing effects of progesterone, is considered the major risk
factor for endometrial cancer and may play a causal role in the development of
the disease. 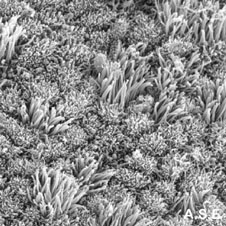
 The uterus has a flat, inner surface and is covered with tall,
columnar epithelial cells. There are pits in the surface that lead down into
uterine glands. The columnar cells, the pits, and the connective tissue and
blood vessels that surround the glands are all part of the endometrium. The
endometrium undergoes dramatic changes during a woman's menstrual cycle. During
the luteal phase, for example, the two-week period just before a woman bleeds,
the endometrium is thick, its epithelial cells are enlarged, the glands bulging,
and the arteries swollen. At menstruation, the arteries break, the epithelial
cells die, and the endometrium, in effect, sheds. Following menstruation, during
the follicular phase, the endometrium regenerates. The changing thickness of the
endometrium is highly dependent on the secretion of oestrogen and progesterone.
Oestrogen causes cellular growth and is an important component of the
rebuilding, follicular phase of the menstrual cycle. Progesterone is secreted
during the later, thick-walled luteal phase, and it balances out the effects of
the oestrogen. Abnormal growth of endometrial cells (whether cancerous or not)
and endometrial cancer are believed to be due to chronic exposure to too much
oestrogen without the balancing effect of progesterone.
The uterus has a flat, inner surface and is covered with tall,
columnar epithelial cells. There are pits in the surface that lead down into
uterine glands. The columnar cells, the pits, and the connective tissue and
blood vessels that surround the glands are all part of the endometrium. The
endometrium undergoes dramatic changes during a woman's menstrual cycle. During
the luteal phase, for example, the two-week period just before a woman bleeds,
the endometrium is thick, its epithelial cells are enlarged, the glands bulging,
and the arteries swollen. At menstruation, the arteries break, the epithelial
cells die, and the endometrium, in effect, sheds. Following menstruation, during
the follicular phase, the endometrium regenerates. The changing thickness of the
endometrium is highly dependent on the secretion of oestrogen and progesterone.
Oestrogen causes cellular growth and is an important component of the
rebuilding, follicular phase of the menstrual cycle. Progesterone is secreted
during the later, thick-walled luteal phase, and it balances out the effects of
the oestrogen. Abnormal growth of endometrial cells (whether cancerous or not)
and endometrial cancer are believed to be due to chronic exposure to too much
oestrogen without the balancing effect of progesterone.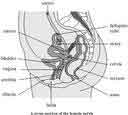 and it does not
invade surrounding tissues or organs, it is considered benign. If the tumour
spreads to surrounding tissues or organs, it is considered malignant, or
cancerous. When cancerous cells break away from the original tumour, travel
through the blood or lymphatic vessels, and grow within other parts of the body,
the process is known as metastasis
and it does not
invade surrounding tissues or organs, it is considered benign. If the tumour
spreads to surrounding tissues or organs, it is considered malignant, or
cancerous. When cancerous cells break away from the original tumour, travel
through the blood or lymphatic vessels, and grow within other parts of the body,
the process is known as metastasis