|
 Hodgkins's
Disease
and
Non-Hodgkins Lymphoma Hodgkins's
Disease
and
Non-Hodgkins Lymphoma
Lymphoma is a cancer
that begins in cells of the immune system. There are two basic
categories of lymphomas. One kind is Hodgkin's lymphoma, which is marked
by the presence of a type of cell called the Reed-Sternberg cell. The
other category is non-Hodgkin's lymphomas, which includes a large,
diverse group of cancers of immune system cells.
Hodgkin's disease (HD) and
non Hodgkin's lymphomas (NHL) - which together are called lymphomas - are
types of cancer. Cancer is not one condition but a word applied to many
different diseases, which have diverse causes and a wide range of
treatments.
The cells which make up our bodies
normally divide in a set and orderly fashion so they can repair our
tissues. This process sometimes goes wrong and there is an uncontrolled
growth of cells. A characteristic of all cancers is this disorderly
formation of body cells, causing swellings or tumours.
A tumour is referred to as benign when
it remains contained in a localised area of the body and, on removal by
surgery, does not recur.
The term cancer is used when the tumours
are malignant i.e. they spread and invade healthy tissue.
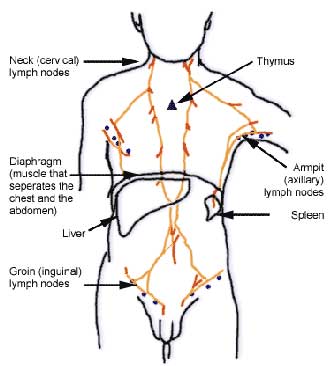
The lymphatic system & lymphomas
The lymphatic system is part of the
body's natural defence against infection. It consists of a wide network of
nodes or glands, which are found all around the body, and are linked by
tiny vessels (or lymphatics).
A clear fluid called lymph circulates
around the body and is drained, via the lymphatics, into the bloodstream.
Lymph contains white blood cells known as lymphocytes. They play a part in
protecting the body from infection. As the lymph circulates through the
lymphatics it is interrupted by the lymph nodes which provide the
opportunity to sieve the lymph and attack invaders.
When the natural division of cells in
the tissues of the lymphatic system become disrupted, tumours called
lymphomas occur. In common with other cancers, lymphomas are not
infectious and cannot be passed on to other people.
The causes of lymphomas are uncertain
but, in some types of lymphoma, research points to a connection with
particular viruses.
There are about 8,000 new cases of
lymphomas diagnosed in Britain each year. Less than a fifth are cases of
Hodgkin's disease, the greater number being non Hodgkin's lymphomas.
Hodgkin's disease
Hodgkin's disease was first identified
by Dr Thomas Hodgkin in 1832. It is characterised by the large
'Reed-Sternberg' cells that may be seen under a microscope when a biopsy
of an affected lymph node, or gland, is studied. The incidence of HD peaks
in the 15 - 30 age group and more men are affected than women.
Nowadays, Hodgkin's disease can be very
successfully treated and many people are completely cured. As the
improvement in treatment is relatively recent - since 1965 - some
textbooks may be out-of-date and thus the information they contain can be
misleading.
Non Hodgkin's lymphoma
There are many different types of non
Hodgkin's lymphomas. Some are so mild that they require little or no
treatment; some are very active. Broadly, NHL is divided into Low Grade
(slow growing) or High Grade (the faster growing lymphomas).
Some consultants refer to a third
category, the Intermediate Grade, which is often considered similar to
High Grade.
Intermediate/High Grade NHL is an
aggressive disease which always needs treatment but it can now be cured in
a fair number of cases.
With Low Grade NHL, although a cure is
not usually possible, the disease can often be controlled for years and
most patients can expect to lead a nearly normal life.
Some rarer forms of lymphomas are hard
to classify as they seem to have some characteristics of both HD and NHL.
NHL is most common in people over 50
years old. It can also arise when the immune system has been suppressed
because of other illnesses or conditions, including organ transplantation.
Symptoms & diagnosis
Often the first symptom is a painless
swelling in one or more of the glands in your neck, armpit, groin or
abdomen. Other symptoms may include:
- night sweats
- fevers
- loss of weight, poor appetite and
tiredness
- a cough or breathlessness
- persistent itch all over
- pain from drinking even a small
quantity of alcohol
On their own, each of these symptoms can
be caused by less serious illnesses. You should consult your GP who will
examine you and decide if further investigation is needed.
Your doctor will refer you to a local
hospital where you will be examined again, before tests take place. These
tests may include:
A biopsy
which is the removal of a small sample of tissue, such as an enlarged
lymph node, for examination under a microscope. This is usually performed
under a general anaesthetic, when you are sent to sleep for about half an
hour or so. Blood samples will show the state of your general
health and how, for example, your kidneys and liver are functioning.
Chest x-rays will be taken to examine your lungs and the lymph glands
in your chest. A bone marrow examination will show if tissue in
this area is affected. The samples will normally be taken from your hip
and the procedure, which takes only a few minutes, is carried out using a
local anaesthetic and it may cause discomfort. Sedation may be offered,
depending on the samples required.
You will probably be asked to undergo a
scan. This can be a CT scan (also known as CAT or body scan) or an MRI
scan or an ultrasound scan of the abdomen. These scans are
painless and take only about an hour, although preparation may be
necessary in advance.
 Occasionally a
lymphangiogram is used. This is a special X-ray of the lymphatic
system, taken after a dye has been injected into your foot. The dye
highlights the lymphatic channels and lymph glands. An overnight stay in
hospital may be required for this test. A dye is also used for anintravenous
urogram (sometimes called an IVU or IVP) but this time it is
injected into a vein in your arm and passes through the bloodstream to
show doctors, via an X-ray, any abnormalities in your kidneys or urinary
system. This test takes place in the X-ray department and lasts about an
hour. Occasionally a
lymphangiogram is used. This is a special X-ray of the lymphatic
system, taken after a dye has been injected into your foot. The dye
highlights the lymphatic channels and lymph glands. An overnight stay in
hospital may be required for this test. A dye is also used for anintravenous
urogram (sometimes called an IVU or IVP) but this time it is
injected into a vein in your arm and passes through the bloodstream to
show doctors, via an X-ray, any abnormalities in your kidneys or urinary
system. This test takes place in the X-ray department and lasts about an
hour.
Such tests are necessary because many
lymph nodes (or glands) in the body cannot be seen or felt, and other
organs must be checked to see if they are affected.
The assessment of what treatment is
required will be based on these tests. You will probably have the results
within 10 - 14 days.
Staging is a system of assessing the
spread of the lymphoma and is one of the factors considered in deciding
your treatment. The stages refer to the parts of the body affected and
also to 'significant symptoms' - namely, the amount of weight loss, fever
and drenching night sweats.
A simplified version of staging is:
Stage 1: one group of lymph nodes (or glands) affected, on one side
of the diaphragm
Stage 2: two or more groups affected, on one side of the diaphragm
Stage 3: lymph nodes (or glands) affected on both sides of the
diaphragm
Stage 4: lymphoma has spread beyond the lymph nodes (or glands) to
other organs such as liver, lungs, bone marrow etc.
The lymphoma is classified as 'B' where
significant symptoms are present and 'A' where there are no significant
symptoms. Therefore, you may hear your doctor refer to your condition as
Stage 1A or Stage 2B and so on.
Even when a lymphoma is suspected,
treatment will usually be delayed until all the tests and staging are
complete. This may be frustrating for you, but a delay of a few weeks
normally has no adverse effects medically and is far better than giving an
inappropriate treatment too early.
Treatment
Your doctor will explain your treatment
timetable. The length of treatment will depend on how well the disease
responds to the drugs but will usually last for several months.
The treatment of each person varies
considerably. The results of your tests, the staging assessment, your age
and general health are all taken into consideration. If the first course
of treatment is not completely successful, there are other possible
treatments.
Hodgkin's disease is treated with
radiotherapy or chemotherapy, or a combination of both.
Intermediate/High Grade NHL is treated
with chemotherapy or a combination of chemotherapy and radiotherapy. If it
is localised it may be treated with radiotherapy alone or, occasionally
surgery.
Low Grade NHL may require no treatment
initially. It may develop slowly and need only mild treatment with
chemotherapy tablets which give few side effects. Sometimes, radiotherapy
and/or intravenous chemotherapy are necessary.
The object of treatment is to cure you,
if this is possible. Where this is not, the aim is to keep the disease
under control and minimise the side effects of treatment. Your quality of
life is very important. However, you may need to accept that the treatment
is sometimes unpleasant but essential in order for you to achieve a normal
life in due course. It is important that you understand what your doctor
is trying to do and that there is confidence between you.
Treatment for other conditions
You should advise your specialist of any
treatment you are having for other conditions, existing or new. Do not
even have a minor operation or dental treatment without telling the doctor
or dentist that you are undergoing treatment for a lymphoma.
Treatment of children
The care and treatment of children
varies from that of adults and is usually undertaken in one of the
specialist children's cancer units. These units have excellent information
and support services for both young patients and their families.
Radiotherapy uses powerful X-rays which are directed onto the cancerous
cells to destroy them, while causing minimal damage to healthy tissue.
Before treatment starts, you will be asked to meet the radiotherapists who
will be supervising your treatment. The area to be treated will be
measured precisely and outlined on your skin using a marker pen.
The machines used to give radiotherapy
vary but some are not dissimilar in appearance to X-ray machines.
Treatment is usually daily, on weekdays, in an outpatient clinic and a
course can last from between 2 - 6 weeks. Your radiographer will position
you on a couch and will protect areas of your body which do not need
treatment. The actual process is painless and lasts only a few minutes.
You will be told how to look after the skin of the treated area and this
is very important. Always ask if you are unsure about any aspect of your
treatment.
Chemotherapy
Chemotherapy means the use of one or
more cytotoxic (anti-cancer) drugs which destroy malignant cells. Often a
combination of four or more drugs is given, normally at intervals of
between one and four weeks.
The drugs are either injected or given
via an intravenous infusion (drip) into a vein, so that they circulate in
the bloodstream throughout the body. Certain drugs may be given as
tablets. Another method is to fit you with a central line (for example a
Portacath or Hickman line). This is a tube which is inserted, after
anaesthetic, into a vein just above your collar bone. It tunnels beneath
your skin and exits through your chest wall. It is used to administer your
drugs and to collect your blood samples.
The effectiveness of the treatment will
be assessed throughout. In most instances, you should be able to have most
of your treatment as an outpatient, but occasionally a night in hospital
may be necessary. Some of the treatment regimens you may hear mentioned
are; CHOP, LOPP, EVAP, Mini BEAM, BEAM, PACEBOM, Ch1Vpp, PABLOE (the
initials refer to the combination of drugs).
Steroids
These are part of your treatment and
have a direct effect on your tumour. They can also help to boost appetite
and energy levels. The downside is that in the short term they may cause
some sleepiness and, if taken over a long time, can give the face a
moon-like appearance and cause weight-gain and sometimes insomnia. Discuss
any problems with your doctor, both when taking steroids and afterwards.
Steroids can make you irritable when you
first take them and depressed for a few days on stopping. Short courses
have very few side effects. Never stop taking steroids suddenly; your
doctor will advise you on reducing them gradually. They are not the same
as anabolic steroids which are banned in sport. Always carry a card
stating that you are taking steroids, in case of emergencies.
Intensive treatment
A small number of people may be treated
with high dose chemotherapy. While 'blitzing' the cancer cells, this
treatment severely suppresses the bone marrow where blood cells are
formed, so patients are also given Autologous Bone Marrow Transplant (ABMT)
or a Peripheral Blood Stem Cell Transplant (PBSCT).
If you have an ABMT, bone marrow is
drawn off under anaesthetic, and stored before chemotherapy starts. After
the intensive treatment, the bone marrow is returned using an intravenous
infusion or drip, rather like a blood transfusion. It will take your bone
marrow some weeks to recover and resume its full role of fighting
infection. For this reason you will have to stay in hospital for 3-6 weeks
until your immune system begins to work again.
With PBSCT, the procedure may start with
a 'priming' dose of chemotherapy plus a growth factor drug to mobilize the
production of stem cells, the primitive cells from which most blood cells
develop. Blood will be taken from you using a machine called a cell
separator. This collects the stem cells, and returns the rest of your
blood to you. This does not involve anaesthetic but does take 3-4 hours.
The collected stem cells are then stored while the main treatment takes
place, and returned via a drip to help the bone marrow recover. Your
recovery time afterwards should, generally, be shorter than for an ABMT.
Non response or recurrence
Occasionally the disease does not
respond to the first treatment used or recurs afterwards. There will be a
number of options. Another treatment will be devised, taking into account
the response to the first, for example, if radiotherapy was used alone,
chemotherapy may be a good second treatment. A different combination of
drugs may be required if chemotherapy has not been successful the first
time, or intensive treatment may be considered.
Infections
Throughout your treatment and during the
period immediately afterwards, you will be very susceptible to infection.
If your spleen has been removed, you are especially vulnerable to certain
infections and should see your doctor immediately at the first sign of
illness.
Most infections arise from bacteria in
your body and cannot be avoided, so tell your specialist if you develop a
sore throat, fevers, unexplained sweats or shivers. Avoid people with infectious diseases,
particularly chickenpox or measles.
Side effects
Your doctor will be able to tell you if
you are likely to have any side effects from your chemotherapy or
radiotherapy. Such side effects are usually temporary and there are ways
of mitigating them. Chemotherapy drugs affect not only lymphoma cells but
also normal cells, especially the ones which multiply fast such as those
in your intestine, hair and bone marrow.
The following table lists the common
side effects and suggests some ways in which they can be minimised.
| |
| Side Effect |
Chemotherapy |
Radiotherapy |
| Nausea & Vomiting |
This will depend on the drugs you are being
given. It can be helpful to keep a diary of when sickness occurs at
home to help your doctor. The newer anti-sickness drugs help prevent
vomiting, but any of these tablets can cause drowsiness, so it may be
inadvisable for you to drive while taking them. |
Any nausea is usually mild, but treatment to
the abdomen can cause problems. |
| Diarrhoea or Constipation |
Each caused by particular drugs. To help, in
either case modify your dietand drink plenty of water. If the problem
persists, ask your doctor or nurse for a prescription. |
You may find either of these a problem if
radiation is given to your abdomen. |
| Sore Mouth |
If you get a sore mouth or mouth ulcers,
these, or white patches, should be shown to your doctor in case
treatment for infection is needed. Special mouthwashes can be given.
You may experience a temporary change in your sense of taste or smell.
A taste caused by the medicine during your injection can be disguised
with a strong sweet. |
If your throat and neck are treated it is
likely to cause difficulty with swallowing and give a dry or sore
mouth. Keeping to a liquid diet and using artificial saliva may help.
Slight changes in taste and sense of smell may persist. |
| Tiredness |
You may expect to be tired during and after
your treatment and this may persist for a time. |
This increases during treatment and you may
find it gets worse for a while after treatment finishes. |
| Neuropathy/Tingling |
Some of the drugs cause tingling in the
fingers and toes. If it becomes really troublesome - so that you have
problems with simple tasks like doing up buttons - tell your doctor. |
|
| Shingles |
This may occur as a result of your disease
or the treatment for it. Pain may occur before the blisters appear.
Tell your doctor early about any new pain, as shingles can now be
effectively treated. Remember that people who have not had chicken
pox, can catch shingles from the chicken pox blister. |
|
| Hair loss |
Only some chemotherapy drugs have this
effect. They can affect the hair on both your head and body, but the
hair will grow again a month to six weeks after you finish treatment. |
Hair will be lost from your head or body
only in the areas being treated. |
|
Research & clinical trials
There is a great deal of research under
way into both the causes and the treatment of lymphomas. The aims of these
studies are to improve the cure rate of lymphomas and reduce the side
effects of treatments.
You may be invited to take part in a
research study or clinical trial, in order that different treatments can
be properly compared. The advantages of taking part in a clinical trial
are that you will be provided with full information, including the
potential benefits, effects and outcomes of the treatment, before coming
to your decision. If you agree to take part in a study, you have the right
to withdraw at any stage and still be treated.
Follow up
After your treatment is complete, you
will be asked to attend follow-up visits at your clinic. You may be given
further tests, similar to those you had at diagnosis. Initially, your
visits will probably be monthly but, if there are no difficulties, the
intervals will gradually lengthen. If any problems arise between
check-ups, let your specialist know as soon as possible. |



