Chemotherapy may be given in different ways, depending on the
type of cancer you have and the chemotherapy drugs used.
Most often it is given by injection into a vein
(intravenously). Some drugs are given as tablets or capsules (orally) and some
are injected into a muscle (intramuscular injection) or just under the skin
(subcutaneous injection). Drugs given in this way are absorbed into the blood
and carried around the body so that they can reach all the cancer cells.
For some types of cancer chemotherapy may be injected into
the fluid around the spine (intrathecal injection). Sometimes the chemotherapy
may be injected into particular body cavities (such as the pelvic cavity or
bladder): this is intra-cavity chemotherapy. Drugs given in this way tend to
stay in the area in which they are given and do not affect cells in other
parts of the body.
Chemotherapy creams may be used for some cancers of the
skin: they only affect the cells in the area to which the cream is applied.
Sometimes, two or more types of chemotherapy may be used
together.
How are chemotherapy drugs given?
- (Most commonly) by injection into a vein
- As tablets or capsules
- By injection into a muscle
- By injection under the skin
- By injection into the fluid around the spine
- By injection into body cavities
- As a cream for cancer of the skin
Intravenous injection
There are 3 main ways of giving chemotherapy drugs directly
into the vein. These are through a:
- cannula - a small tube inserted into a vein in your arm
or the back of your hand.
-
central line - a thin, flexible
tube inserted through the skin of the chest into a vein near · the heart.
-
PICC line (a peripherally inserted
central line) -- a thin flexible tube is passed into a vein in the crook of
your arm and then threaded through until the end of the tube lies in a vein
near the heart.
- portocath - a portocath is also called an
implantable port and is a thin, soft plastic tube that is put into a
vein. It has an opening (port) just under the skin on your chest or arm.
Cannula
The nurse or doctor will put a short, fine tube (cannula)
into a vein in the back of your hand or the crook of your arm. You may find
this uncomfortable or a little painful but it should not take long. Once the
cannula is in place it will be taped securely to keep it in place.
If you find it painful to have the cannula put in, an
anaesthetic cream can be used on the skin to numb the area beforehand. The
cream takes 10-20 minutes to work.
The chemotherapy can then be given through the cannula.
Usually a drip is attached to the cannula and some drugs are given by
injection into a rubber bung in the drip tubing. This can take from a few
minutes to about 20 minutes. Some chemotherapy drugs are diluted in a drip bag
and the drip is attached to the cannula.
If you feel any discomfort or a change in sensation around
the area of the cannula while the drug is being given, let your nurse or
doctor know immediately.
Central lines
Another way of giving intravenous chemotherapy is through a
long, fine plastic tube (called a central line) put into a vein in your chest.
Hickman or Groshong lines are common types. The doctor or chemotherapy nurse
will explain the procedure to you. You will be given a general or local
anaesthetic before the central line is put in.
- Central line is inserted into your chest here
- The line is tunnelled under your skin
- It comes out here
Once it is in place, the central line is either stitched or
taped firmly to your chest to prevent it being pulled out of the vein. It can
remain in the vein for many months and means that you do not have to have
cannulas put in when you have your intravenous chemotherapy. Blood can also be
taken through this line for testing.
You will be able to bathe or shower; although you should
prevent water from getting to the area where the tube enters the skin - a
plastic dressing can be used for this.
There are very few restrictions to everyday life. Before you
go home, make sure you are confident about looking after your central line. If
you do have any problems, contact the staff on the ward for advice.
Possible problems with central lines
Two potential problems with central lines are blockage and
infection. Once or twice a week the line has to be flushed with heparin, a
drug which prevents clotting, and the nurses on the ward can teach you how to
do this.
If you notice any reddening, darkening or soreness of the
skin around the central line, or if you have a high temperature, let your
doctor know as it could be a sign that you have an infection in the line. If
this happens you will need to have antibiotics through the line to clear the
infection.
Most hospitals consider a temperature above 38°C (100.5°F)
to be high, but some hospitals use a lower or higher temperature. The doctors
and nurses at your hospital will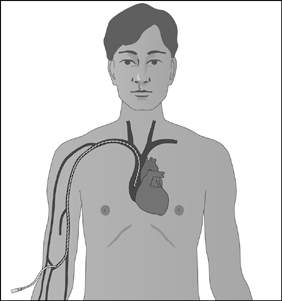 tell you which temperature they use.
tell you which temperature they use.
PICC lines
Your doctor may decide to put a long, fine line into a vein
in the crook of your arm. This is called a peripherally inserted central
venous catheter (PICC). The doctor or chemotherapy nurse will explain the
procedure to you. You will be given a local anaesthetic before the line is put
in. The tube is threaded through the vein until the end is near
to your heart.
The end of the tube comes out just below the
crook of your elbow.
Once it is in place, the PICC line is taped firmly to your
arm to prevent it being pulled out of the vein. It can remain in the vein for
many months. As with the central line it means that you do not have to have
cannulas put in when you have your intravenous chemotherapy. Blood can also be
taken through the line for testing.
You will be able to bathe or shower, although you should
prevent water from getting to the area around the tube - a plastic dressing
can be used for this.
There are very few restrictions to everyday life. Before you
go home, make sure that you are confident about looking after your line. If
you do have any problems contact the staff on the ward for advice.
The possible problems are the same as for central lines:
blockage and infection
Portocaths (implantable ports)
An implantable port is a thin, soft plastic tube that is put
into a vein and has an opening (port) just under the skin on your chest or
arm. This allows medicines to be given into the vein or blood to be taken from
the vein.
The tube is a long, thin hollow tube known as a catheter and
the port is a disc about 2.5 to 4 cm in diameter. The catheter is usually
inserted (tunnelled) under the skin of your chest. The tip of the catheter
lies in a large vein just above your heart and the other end connects with the
port which sits under the skin on your upper chest. The port will show as a
small bump underneath your skin which can be felt, but nothing is visible on
the outside of your body.
Infusion pumps
Infusion pumps may be used to give some types of
chemotherapy. There are various types of portable pump. These can be used to
give a controlled amount of drugs into the bloodstream over a period of time
(from a few days to a few weeks).
The pump is connected to a central line or a PICC line. This
means that you can go home with the pump and so you need fewer visits to
hospital. The pumps are small enough to be carried in a bag or belt holster.
 The chemotherapy drugs are prepared at the hospital. You,
and perhaps a family member or friend, will be taught how to look after the
pump. Some pumps are battery-operated and care has to be taken not to get them
wet when you are washing (the nurses will give you full instructions).
The chemotherapy drugs are prepared at the hospital. You,
and perhaps a family member or friend, will be taught how to look after the
pump. Some pumps are battery-operated and care has to be taken not to get them
wet when you are washing (the nurses will give you full instructions).
Some pumps are disposable after use and are operated by a
balloon mechanism or spring control.
Chemotherapy tablets or capsules
You may be given tablets or capsules to take at home as all
or part of your treatment. Tablets or capsules are known as oral chemotherapy.
You will be told when to take them and will be given other instructions such
as whether or not to take them with food.
If you cannot take your medicines for any reason you should
contact your doctor immediately for advice. The drugs that you have been given
by the hospital make up a complete course of treatment, and it is important to
take them exactly as they have been prescribed.
If you need to have further supplies of the drug it is
important to get these from your hospital specialist and not from your GP or
local pharmacist.
Intramuscular injection
Some chemotherapy drugs are given by injection into a
muscle. The doctor or nurse will explain the procedure to you. The drug is
injected into the muscle of the leg or buttock. This may be painful or
uncomfortable, but only lasts for a short time.
Subcutaneous injection
Some drugs can be given by injection just under the skin. A
very fine needle is used and this may be uncomfortable for a short time.
Intrathecal injection (into the fluid around the spinal
cord)
In some conditions such as leukaemia or lymphoma (cancer
which starts in the lymph system) cancer cells can pass into the fluid which
surrounds the brain and spinal cord. The fluid is known as cerebrospinal fluid
or CSF.
To prevent this from happening, or to treat it if it occurs,
chemotherapy may be given into the CSF. To do this you need to lie on your
side with your legs drawn up. The doctor will then use local anaesthetic to
numb an area of skin over your spine. A needle is then inserted into the space
between two of the spinal bones and into the CSF. The chemotherapy is injected
into the CSF through the needle.
This procedure takes from 15 to 30 minutes and you may need
to lie flat afterwards for a few hours. You may have a headache, which will
last for a few hours. Painkillers can be given for this. Chemotherapy given in
this way does not usually cause any other side effects.
Intra-cavity chemotherapy
To give chemotherapy drugs in this way a tube is inserted
into the affected body cavity, for example the bladder, and the chemotherapy
is flushed in through the tube. It may then be drained out again after a set
period of time.
Drugs given in this way may cause some irritation or
inflammation in the area to which they are given but they do not tend to cause
side effects in other parts of the body.
Chemotherapy creams
Chemotherapy creams are used for some types of skin cancer.
They are put on to the affected area of skin in a thin layer and may need to
be used regularly for a few weeks. They may cause some soreness or irritation
of the skin in the affected area but do not cause side effects in other parts
of the body.
While you are using chemotherapy creams you may need to wear
a dressing over the affected area of skin.
SIDE EFFECTS